

Dec 30, 2025
Dec 30, 2025
Guide to Climate-Resilient Health Systems
Capacity Building
Capacity Building
In This Article
Health systems must assess climate risks, strengthen infrastructure, and use early warning and monitoring to keep medical services running during extreme weather.
Guide to Climate-Resilient Health Systems
The increasing frequency of extreme weather events like hurricanes, floods, and heat waves is putting healthcare systems under immense pressure. Climate-resilient health systems are designed to remain functional during such crises, ensuring uninterrupted medical services and support for communities. This guide outlines actionable steps, including conducting risk assessments, building robust infrastructure, and integrating early warning systems, to help healthcare facilities prepare for climate challenges.
Key Takeaways:
Risk Assessments: Identify threats using tools like the U.S. Climate Resilience Toolkit and WHO checklists.
Infrastructure Planning: Design facilities with future climate risks in mind, ensuring energy and water redundancy.
Surveillance and Monitoring: Use real-time systems to track and address climate-sensitive health risks.
Early Warning Systems: Develop protocols to maintain critical services during disruptions.
Collaboration: Work with local agencies, emergency teams, and community stakeholders for a coordinated response.
Start by mapping vulnerabilities, integrating climate and health data, and creating a resilience plan tailored to your facility’s needs. These strategies ensure healthcare systems can withstand and recover from climate-related disruptions while continuing to serve their communities effectively.
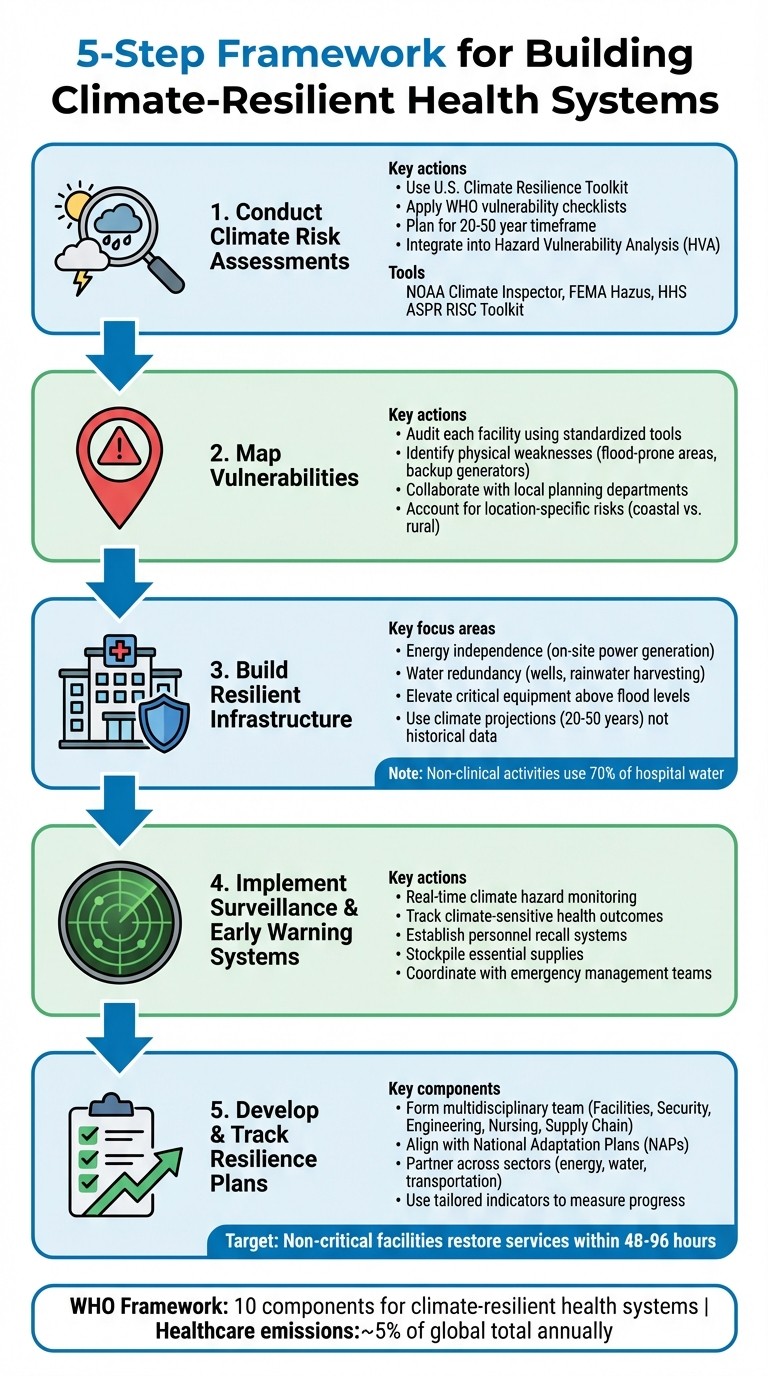
5-Step Framework for Building Climate-Resilient Health Systems
Building Climate-Resilient Health Systems
Conducting Climate Risk Assessments
To build resilience, healthcare systems first need to pinpoint potential threats through comprehensive climate risk assessments. These evaluations should account for both gradual changes, like rising sea levels, and sudden events, such as hurricanes or heat waves [6]. The U.S. Climate Resilience Toolkit highlights the importance of this process:
Health care organizations are encouraged to conduct a climate risk assessment so that they may better understand and catalog present and future extreme weather risks [6].
Such assessments are vital for long-term planning, typically spanning 20 to 50 years, and should be integrated into an organization's broader Hazard Vulnerability Analysis (HVA). This ensures a well-rounded, multi-hazard approach [6]. Once risks are identified, the next step is to map specific vulnerabilities at each facility to address these threats effectively.
How to Map Vulnerabilities
Mapping vulnerabilities requires a tailored approach, as risks vary significantly by location. For example, hospitals along Florida’s coast face threats like hurricanes and flooding, while facilities in rural Montana might contend with harsh winters or limited access to resources. Rural hospitals often serve as community hubs during emergencies, providing food, water, and shelter, whereas urban centers may focus on specialized medical care [6].
Begin by auditing each facility using standardized tools like the WHO "Checklists to Assess Vulnerabilities in Health Care Facilities" or the HHS "Climate Resilience Checklists." These tools help identify physical weaknesses, such as critical equipment located in flood-prone areas or backup generators that might fail under extreme heat [4][7]. Collaborate with local planning departments, municipal authorities, and community stakeholders to ensure your assessment aligns with regional climate projections [6]. If interpreting climate models proves challenging, consider partnering with local universities or sustainability consulting for expert guidance [6].
Combining Climate and Health Data
Once vulnerabilities are mapped, the next step is to integrate climate projections with health data. This combination provides a fuller picture of where impacts will hit hardest. Overlaying climate data with health statistics, disease prevalence, and socioeconomic factors helps identify populations most at risk [7]. The WHO underscores the value of this approach:
Vulnerability and Adaptation Assessments (V&As) are a key instrument to identify and prepare for changing health risks. V&A assessments can provide information for decision-makers on the extent and magnitude of likely health risks attributable to climate change [7].
This integration enables health systems to anticipate how climate shifts will influence disease patterns. For instance, rising temperatures could expand the range of mosquito-borne illnesses or accelerate pathogen incubation periods. By merging temperature projections with current disease surveillance, healthcare organizations can predict emerging health threats and allocate resources to areas of greatest need.
Predictive Tools and Frameworks
Several tools are available to simplify climate risk assessments. NOAA's Climate Inspector delivers localized projections for temperature and precipitation [6]. FEMA's Hazus software estimates potential losses from disasters like floods, hurricanes, and earthquakes [6]. The HHS ASPR RISC Toolkit (Risk Identification and Site Criticality) helps healthcare facilities identify risks and improve emergency preparedness [4]. For coastal areas, the Coastal Flood Exposure Mapper visualizes flooding risks, while CanVis offers photo-edited simulations of how sea-level rise could impact specific sites [6]. These tools allow healthcare systems to better prepare for and mitigate climate-driven disruptions.
These resources are part of larger frameworks, such as the WHO Operational Framework for Building Climate Resilient Health Systems. This framework includes 10 components, with risk assessment as a central element [7][8]. It also emphasizes the importance of addressing healthcare systems' own greenhouse gas emissions, which account for roughly 5% of global emissions annually [7]. By leveraging these tools and frameworks, healthcare organizations can take meaningful steps toward climate resilience.
Core Components of Climate-Resilient Health Systems
After identifying risks, healthcare organizations need to focus on the essential elements that ensure facilities remain functional during climate emergencies. These components work together to safeguard both infrastructure and patient care when extreme weather events occur.
Building Resilient Infrastructure
Strong infrastructure is the backbone of climate resilience. According to the U.S. Department of Health and Human Services:
Essential health services must remain available to communities and individuals during and immediately following extreme weather events, even during extended utility outages and transportation infrastructure disturbances. [5]
A major focus is energy independence. Facilities can boost resilience by adopting on-site power generation systems, such as Combined Heat and Power systems, which allow them to function even if the regional power grid fails. To further protect critical systems, fuel pumps, tanks, and electrical switchgear should be positioned above anticipated flood levels to reduce the risk of damage.
Water redundancy is another priority. On-site wells, rainwater harvesting systems, and reclaimed water solutions can ensure a steady supply. With non-clinical activities consuming up to 70% of hospital water [5], reclaimed systems can help maintain operations while easing the strain on municipal resources.
Infrastructure planning should also shift away from outdated historical data and instead rely on climate projections for the next 20 to 50 years. This forward-thinking approach can guide the design of roads, stormwater systems, and building structures to better withstand future conditions. Nature-based solutions, like advanced stormwater management and strategies to mitigate urban heat islands, can complement these efforts by supporting natural water flow and adding extra layers of protection.
Physical upgrades alone are not enough - real-time data and monitoring systems are essential for ensuring operational readiness.
Improving Surveillance and Monitoring
Real-time surveillance systems allow health facilities to anticipate and address climate-related risks before they escalate. Monitoring climate hazards and understanding community vulnerabilities not only aids immediate service delivery but also informs long-term planning. By tracking climate-sensitive health outcomes across different regions, these systems can pinpoint populations at the highest risk.
Advanced technologies can enhance these monitoring efforts. For example, integrating climate risk assessments into existing Hazard Vulnerability Analysis enables data-driven planning. This helps facilities prepare for patient surges and manage shelter-in-place scenarios for those with medical vulnerabilities.
Once robust surveillance systems are in place, they lay the groundwork for effective early warning responses.
Creating Early Warning and Response Systems
Early warning systems are crucial for activating response protocols that keep essential clinical services - such as emergency departments, imaging facilities, and laboratories - operational during and after extreme weather events. These systems rely on earlier risk assessments to trigger timely actions.
Effective response planning also hinges on clear personnel coordination. Facilities should establish recall systems in collaboration with local and regional emergency management teams to ensure medical and support staff can either reach the facility or remain on-site during transportation disruptions. Stockpiling essential supplies on-site further bolsters the ability to operate during extended disruptions to supply chains.
Early warning indicators, which can provide timelines ranging from weeks to years, give healthcare systems the ability to scale up capacity, secure backup resources, and work proactively with community partners to manage potential challenges.
Creating Climate Resilience Plans
Once vulnerabilities are mapped and resilient infrastructure is established, the next step is crafting a resilience plan. This plan brings previous risk assessments into action, ensuring uninterrupted services during climate-related events.
Planning Steps
Start with a Hazard Vulnerability Assessment (HVA) using tools like the RISC Toolkit to identify risks and critical facilities [4]. Build the plan around five key elements:
Updated Data: Incorporate the latest climate hazard and vulnerability information.
Resilient Design: Use land planning and building designs that anticipate future weather extremes.
Secured Systems: Establish energy, water, and waste systems designed to withstand extreme events throughout their entire lifespan [3].
Clinical Care Protocols: Develop procedures for maintaining essential care during patient surges, including sheltering in place when transportation is unavailable.
Environmental Measures: Implement green infrastructure and strategies to reduce heat islands across your campus [3].
For non-critical facilities, ensure plans allow for safe closures and quick service resumption within 48–96 hours [3].
Form a multidisciplinary team that includes members from Facilities, Security, Engineering, Nursing, Supply Chain, Emergency Planning, and other relevant departments. This ensures a thorough approach to planning [3]. Standardized tools, like the Sustainable and Climate-Resilient Health Care Facilities Toolkit, can help transform assessments into actionable strategies [3].
Working with Stakeholders
Use insights from your vulnerability maps to engage with local agencies and community leaders. Collaborate with emergency preparedness teams, public health officials, and other stakeholders - such as those in water, sanitation, and nutrition sectors - to address risks beyond your facility [9][4]. International development agencies can also direct investments toward strengthening public health systems [9].
Your resilience plan should align with broader frameworks like National Adaptation Plans (NAPs) under the UN Framework Convention on Climate Change [9]. The World Health Organization highlights that resilience planning goes beyond infrastructure. It involves activities, partnerships, and the collective capacity of various actors within the health system [1]. Tailor specific indicators to track progress rather than relying on generic metrics, and integrate your efforts with existing health surveillance systems to avoid redundancy [1].
How Council Fire Supports Climate Resilience Planning
Expert guidance can turn even the most comprehensive plans into actionable strategies. Council Fire offers a systems-based approach to climate resilience planning, focusing on translating sustainability goals into measurable outcomes. Their expertise ensures organizations move beyond simple compliance, enabling them to create meaningful progress through data-driven insights and stakeholder-focused planning.
Council Fire’s services combine technical know-how with strategic communication, ensuring infrastructure is prepared for future challenges while addressing environmental, social, and economic goals. Their approach includes in-depth impact analysis, fostering trust through stakeholder engagement, and crafting communication strategies that inspire organizational change around sustainability.
Policy Development and Implementation
Incorporating climate considerations into health policies and daily operations is essential for creating resilient health systems. The WHO Operational Framework outlines 10 key components to guide this process [8][2]. By building on existing Hazard Vulnerability Analysis (HVA) processes, organizations can ensure climate resilience becomes a standard practice rather than an afterthought [5]. This approach forms a strong basis for integrating these considerations into cohesive health strategies.
Integrating Climate into Health Policies
Health policies should align with global frameworks such as National Adaptation Plans (NAPs), Universal Health Coverage, and the Sustainable Development Goals [8][2]. Infrastructure standards must also be updated to account for climate projections over the next 20–50 years, ensuring preparedness for future challenges [5]. Modern health systems must aim to be both climate-resilient and low-carbon [2].
"Failure to prepare for climate change now by bolstering the resilience of health systems increases the probability that hazards become disasters and complex emergencies that cause severe impacts to human health and communities."
WHO [1]
To ensure policies are practical and actionable, a multi-disciplinary team should be formed. This team might include representatives from Facilities, Security, Engineering, Nursing, Supply Chain, and Emergency Planning, ensuring that policies reflect operational realities [5].
Partnering Across Sectors
Health systems cannot achieve resilience in isolation. Collaboration with sectors such as energy, water, transportation, and emergency management is crucial to maintaining essential services during prolonged utility outages [5]. These sectors, often referred to as "health-determining sectors", play a direct role in ensuring care delivery during climate-related events [8][1]. For instance, formal Emergency Water Supply Plans should be developed to evaluate water usage, response capabilities, and alternative supply options like on-site wells or rainwater harvesting [5].
Beyond infrastructure, partnerships should include experts in nutrition and sanitation to address risks like food insecurity and waterborne diseases that are exacerbated by climate variability [8]. Once these cross-sector collaborations are in place, tracking progress becomes vital to ensuring effectiveness.
Tracking Progress and Results
"Measuring the climate resilience of a health system is most effectively done with information and indicators that are tailored to the needs of the health authority using it."
WHO [1]
To effectively measure progress, health systems should use indicators that address local health concerns rather than relying solely on broad international metrics [1]. Leveraging existing national health surveillance and monitoring infrastructure can help avoid redundancy [1]. It’s important to evaluate the system’s ability to anticipate, respond to, recover from, and adapt to climate-related challenges [1]. Tools such as the HHS ASPR Risk Identification and Site Criticality (RISC) Toolkit can provide baseline assessments, while the Climate Resilience for Health Care toolkit aids in integrating climate considerations into emergency preparedness plans [4].
Progress tracking should cover both health outcomes and the resilience of supporting infrastructure across various activities and actors within the health system [1]. Metrics should also include greenhouse gas emission reductions alongside resilience indicators to assess progress toward low-carbon operations [2]. For multi-campus health systems, site-specific assessments are essential, as risks and vulnerabilities can vary widely based on location and climate zone [5].
Conclusion and Key Takeaways
Building climate-resilient health systems is essential for safeguarding communities and ensuring uninterrupted care during extreme weather events. The strategies outlined here provide a structured approach for health organizations to address climate challenges while maintaining their ability to serve effectively.
Main Strategies Recap
Achieving climate resilience involves addressing both immediate vulnerabilities and long-term adaptation needs. Start with a detailed vulnerability assessment that combines climate projections with health data. From there, focus on creating resilient infrastructure by:
Assessing climate risks and considering future extremes in land use and building design.
Implementing sustainable energy and water solutions to protect critical systems.
Ensuring essential clinical services remain operational during disruptions.
Incorporating environmental protections like green infrastructure to mitigate risks.
As emphasized, integrating risk assessments with resilient design and fostering collaboration across sectors is vital for long-term success.
Collaboration with sectors such as energy, water, transportation, and emergency management is crucial for maintaining essential services during extended outages. Facilities that are less critical should aim to restore services within 48 to 96 hours after a major weather event [3].
To measure progress, use customized indicators that evaluate your system's capacity to anticipate, respond to, recover from, and adapt to climate-related challenges. These strategies offer a clear path for immediate and practical action.
Next Steps
Begin by conducting a standardized vulnerability assessment to identify weaknesses in infrastructure, communication systems, and supply chains. Instead of creating separate initiatives, integrate climate considerations into your existing emergency preparedness plans - resilience efforts are most effective when embedded into established processes.
Consider collaborating with experts who specialize in both sustainability and health system operations. For instance, Council Fire provides strategic guidance and actionable plans to help organizations build climate resilience. They focus on sustainable infrastructure, energy and water systems, and cross-sector partnerships, enabling health systems to balance environmental considerations with operational continuity. Their expertise can help accelerate progress toward a climate-resilient future while ensuring your health system remains dependable when your community needs it most.
FAQs
What makes a health system climate-resilient?
A climate-resilient health system is built to handle the growing challenges posed by climate change, such as extreme heat, floods, storms, and wildfires, while actively working to lower its own greenhouse gas (GHG) emissions. According to the World Health Organization, achieving this requires ten essential components, including effective governance, a skilled workforce, comprehensive climate risk assessments, and infrastructure designed with sustainability in mind.
These systems emphasize real-time monitoring, health programs tailored to climate realities, and strong emergency preparedness to safeguard communities from climate-related threats. Equally important are sustainable funding models and the use of advanced, climate-conscious technologies to ensure long-term resilience.
In the U.S., Council Fire supports health organizations in adopting these strategies. By providing expertise in areas like sustainable infrastructure, energy systems, and stakeholder collaboration, they help align climate initiatives with broader financial and social goals.
How can healthcare facilities identify and address climate-related risks effectively?
To tackle climate-related risks effectively, healthcare facilities must start by evaluating their unique vulnerabilities. This means collecting up-to-date, location-specific climate data to understand potential threats like floods, heat waves, wildfires, or rising sea levels. Facilities should then analyze how these risks could impact their infrastructure, utilities, and service areas. Tools like mapping software can be particularly useful for visualizing high-risk zones and pinpointing critical systems - such as power supplies or water infrastructure - that might be disrupted during extreme weather events.
After identifying these risks, prioritization is key. Facilities should rank threats based on their likelihood, the potential impact on essential services, and the specific needs of the community they serve. Practical steps might include installing backup generators, reinforcing building structures, and ensuring supply chains remain reliable under adverse conditions. Collaboration with stakeholders - such as staff, emergency managers, and local community members - can ensure solutions are both effective and tailored to the community's context.
Council Fire offers healthcare providers strategic support in assessing risks, planning, and implementing climate-resilient measures. By weaving these efforts into routine planning, healthcare systems can safeguard patient care while bolstering community resilience against climate-related challenges.
How do early warning systems help healthcare facilities prepare for extreme weather events?
Early warning systems are indispensable for keeping healthcare facilities operational during extreme weather events. By delivering timely alerts about potential threats like floods, heat waves, storms, or power outages, these systems enable hospitals, clinics, and long-term care facilities to take precautionary measures. Actions might include securing backup power sources, safeguarding critical medical equipment, pre-stocking necessary supplies, and organizing safe transportation for both staff and patients.
Incorporating early warning data into risk assessments allows healthcare organizations to better prepare for climate-related challenges over time. This approach strengthens both infrastructure and operations, ensuring greater resilience. Additionally, these systems facilitate the swift implementation of response protocols, such as activating shelter plans, establishing evacuation routes, and coordinating with community support networks. The result is minimized disruptions and enhanced safety for patients and healthcare workers alike.
Council Fire supports healthcare systems in integrating early warning capabilities into their emergency strategies, fostering coordinated efforts to maintain care delivery even during severe weather conditions.
Related Blog Posts

Latest Articles
©2025
FAQ
FAQ
01
What does it really mean to “redefine profit”?
02
What makes Council Fire different?
03
Who does Council Fire you work with?
04
What does working with Council Fire actually look like?
05
How does Council Fire help organizations turn big goals into action?
06
How does Council Fire define and measure success?
01
What does it really mean to “redefine profit”?
02
What makes Council Fire different?
03
Who does Council Fire you work with?
04
What does working with Council Fire actually look like?
05
How does Council Fire help organizations turn big goals into action?
06
How does Council Fire define and measure success?


Dec 30, 2025
Guide to Climate-Resilient Health Systems
Capacity Building
In This Article
Health systems must assess climate risks, strengthen infrastructure, and use early warning and monitoring to keep medical services running during extreme weather.
Guide to Climate-Resilient Health Systems
The increasing frequency of extreme weather events like hurricanes, floods, and heat waves is putting healthcare systems under immense pressure. Climate-resilient health systems are designed to remain functional during such crises, ensuring uninterrupted medical services and support for communities. This guide outlines actionable steps, including conducting risk assessments, building robust infrastructure, and integrating early warning systems, to help healthcare facilities prepare for climate challenges.
Key Takeaways:
Risk Assessments: Identify threats using tools like the U.S. Climate Resilience Toolkit and WHO checklists.
Infrastructure Planning: Design facilities with future climate risks in mind, ensuring energy and water redundancy.
Surveillance and Monitoring: Use real-time systems to track and address climate-sensitive health risks.
Early Warning Systems: Develop protocols to maintain critical services during disruptions.
Collaboration: Work with local agencies, emergency teams, and community stakeholders for a coordinated response.
Start by mapping vulnerabilities, integrating climate and health data, and creating a resilience plan tailored to your facility’s needs. These strategies ensure healthcare systems can withstand and recover from climate-related disruptions while continuing to serve their communities effectively.
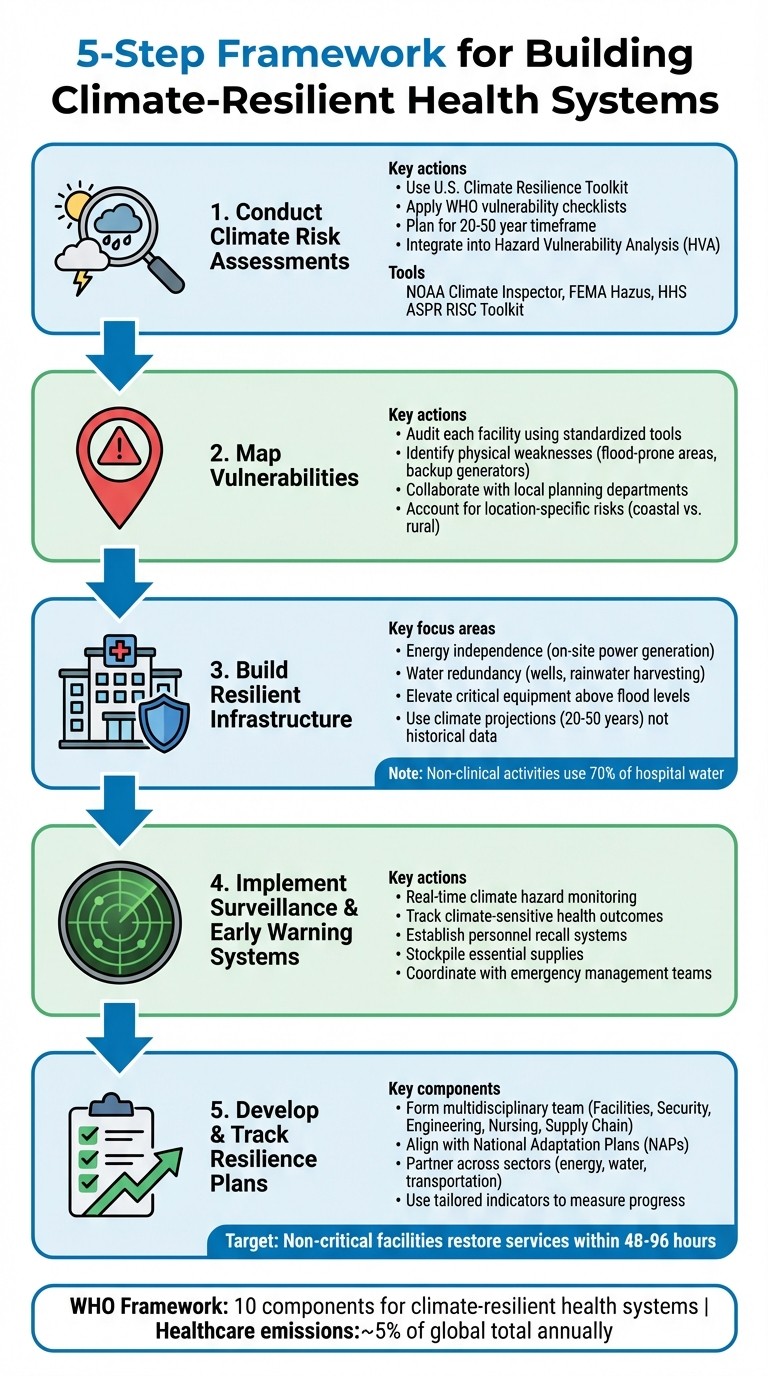
5-Step Framework for Building Climate-Resilient Health Systems
Building Climate-Resilient Health Systems
Conducting Climate Risk Assessments
To build resilience, healthcare systems first need to pinpoint potential threats through comprehensive climate risk assessments. These evaluations should account for both gradual changes, like rising sea levels, and sudden events, such as hurricanes or heat waves [6]. The U.S. Climate Resilience Toolkit highlights the importance of this process:
Health care organizations are encouraged to conduct a climate risk assessment so that they may better understand and catalog present and future extreme weather risks [6].
Such assessments are vital for long-term planning, typically spanning 20 to 50 years, and should be integrated into an organization's broader Hazard Vulnerability Analysis (HVA). This ensures a well-rounded, multi-hazard approach [6]. Once risks are identified, the next step is to map specific vulnerabilities at each facility to address these threats effectively.
How to Map Vulnerabilities
Mapping vulnerabilities requires a tailored approach, as risks vary significantly by location. For example, hospitals along Florida’s coast face threats like hurricanes and flooding, while facilities in rural Montana might contend with harsh winters or limited access to resources. Rural hospitals often serve as community hubs during emergencies, providing food, water, and shelter, whereas urban centers may focus on specialized medical care [6].
Begin by auditing each facility using standardized tools like the WHO "Checklists to Assess Vulnerabilities in Health Care Facilities" or the HHS "Climate Resilience Checklists." These tools help identify physical weaknesses, such as critical equipment located in flood-prone areas or backup generators that might fail under extreme heat [4][7]. Collaborate with local planning departments, municipal authorities, and community stakeholders to ensure your assessment aligns with regional climate projections [6]. If interpreting climate models proves challenging, consider partnering with local universities or sustainability consulting for expert guidance [6].
Combining Climate and Health Data
Once vulnerabilities are mapped, the next step is to integrate climate projections with health data. This combination provides a fuller picture of where impacts will hit hardest. Overlaying climate data with health statistics, disease prevalence, and socioeconomic factors helps identify populations most at risk [7]. The WHO underscores the value of this approach:
Vulnerability and Adaptation Assessments (V&As) are a key instrument to identify and prepare for changing health risks. V&A assessments can provide information for decision-makers on the extent and magnitude of likely health risks attributable to climate change [7].
This integration enables health systems to anticipate how climate shifts will influence disease patterns. For instance, rising temperatures could expand the range of mosquito-borne illnesses or accelerate pathogen incubation periods. By merging temperature projections with current disease surveillance, healthcare organizations can predict emerging health threats and allocate resources to areas of greatest need.
Predictive Tools and Frameworks
Several tools are available to simplify climate risk assessments. NOAA's Climate Inspector delivers localized projections for temperature and precipitation [6]. FEMA's Hazus software estimates potential losses from disasters like floods, hurricanes, and earthquakes [6]. The HHS ASPR RISC Toolkit (Risk Identification and Site Criticality) helps healthcare facilities identify risks and improve emergency preparedness [4]. For coastal areas, the Coastal Flood Exposure Mapper visualizes flooding risks, while CanVis offers photo-edited simulations of how sea-level rise could impact specific sites [6]. These tools allow healthcare systems to better prepare for and mitigate climate-driven disruptions.
These resources are part of larger frameworks, such as the WHO Operational Framework for Building Climate Resilient Health Systems. This framework includes 10 components, with risk assessment as a central element [7][8]. It also emphasizes the importance of addressing healthcare systems' own greenhouse gas emissions, which account for roughly 5% of global emissions annually [7]. By leveraging these tools and frameworks, healthcare organizations can take meaningful steps toward climate resilience.
Core Components of Climate-Resilient Health Systems
After identifying risks, healthcare organizations need to focus on the essential elements that ensure facilities remain functional during climate emergencies. These components work together to safeguard both infrastructure and patient care when extreme weather events occur.
Building Resilient Infrastructure
Strong infrastructure is the backbone of climate resilience. According to the U.S. Department of Health and Human Services:
Essential health services must remain available to communities and individuals during and immediately following extreme weather events, even during extended utility outages and transportation infrastructure disturbances. [5]
A major focus is energy independence. Facilities can boost resilience by adopting on-site power generation systems, such as Combined Heat and Power systems, which allow them to function even if the regional power grid fails. To further protect critical systems, fuel pumps, tanks, and electrical switchgear should be positioned above anticipated flood levels to reduce the risk of damage.
Water redundancy is another priority. On-site wells, rainwater harvesting systems, and reclaimed water solutions can ensure a steady supply. With non-clinical activities consuming up to 70% of hospital water [5], reclaimed systems can help maintain operations while easing the strain on municipal resources.
Infrastructure planning should also shift away from outdated historical data and instead rely on climate projections for the next 20 to 50 years. This forward-thinking approach can guide the design of roads, stormwater systems, and building structures to better withstand future conditions. Nature-based solutions, like advanced stormwater management and strategies to mitigate urban heat islands, can complement these efforts by supporting natural water flow and adding extra layers of protection.
Physical upgrades alone are not enough - real-time data and monitoring systems are essential for ensuring operational readiness.
Improving Surveillance and Monitoring
Real-time surveillance systems allow health facilities to anticipate and address climate-related risks before they escalate. Monitoring climate hazards and understanding community vulnerabilities not only aids immediate service delivery but also informs long-term planning. By tracking climate-sensitive health outcomes across different regions, these systems can pinpoint populations at the highest risk.
Advanced technologies can enhance these monitoring efforts. For example, integrating climate risk assessments into existing Hazard Vulnerability Analysis enables data-driven planning. This helps facilities prepare for patient surges and manage shelter-in-place scenarios for those with medical vulnerabilities.
Once robust surveillance systems are in place, they lay the groundwork for effective early warning responses.
Creating Early Warning and Response Systems
Early warning systems are crucial for activating response protocols that keep essential clinical services - such as emergency departments, imaging facilities, and laboratories - operational during and after extreme weather events. These systems rely on earlier risk assessments to trigger timely actions.
Effective response planning also hinges on clear personnel coordination. Facilities should establish recall systems in collaboration with local and regional emergency management teams to ensure medical and support staff can either reach the facility or remain on-site during transportation disruptions. Stockpiling essential supplies on-site further bolsters the ability to operate during extended disruptions to supply chains.
Early warning indicators, which can provide timelines ranging from weeks to years, give healthcare systems the ability to scale up capacity, secure backup resources, and work proactively with community partners to manage potential challenges.
Creating Climate Resilience Plans
Once vulnerabilities are mapped and resilient infrastructure is established, the next step is crafting a resilience plan. This plan brings previous risk assessments into action, ensuring uninterrupted services during climate-related events.
Planning Steps
Start with a Hazard Vulnerability Assessment (HVA) using tools like the RISC Toolkit to identify risks and critical facilities [4]. Build the plan around five key elements:
Updated Data: Incorporate the latest climate hazard and vulnerability information.
Resilient Design: Use land planning and building designs that anticipate future weather extremes.
Secured Systems: Establish energy, water, and waste systems designed to withstand extreme events throughout their entire lifespan [3].
Clinical Care Protocols: Develop procedures for maintaining essential care during patient surges, including sheltering in place when transportation is unavailable.
Environmental Measures: Implement green infrastructure and strategies to reduce heat islands across your campus [3].
For non-critical facilities, ensure plans allow for safe closures and quick service resumption within 48–96 hours [3].
Form a multidisciplinary team that includes members from Facilities, Security, Engineering, Nursing, Supply Chain, Emergency Planning, and other relevant departments. This ensures a thorough approach to planning [3]. Standardized tools, like the Sustainable and Climate-Resilient Health Care Facilities Toolkit, can help transform assessments into actionable strategies [3].
Working with Stakeholders
Use insights from your vulnerability maps to engage with local agencies and community leaders. Collaborate with emergency preparedness teams, public health officials, and other stakeholders - such as those in water, sanitation, and nutrition sectors - to address risks beyond your facility [9][4]. International development agencies can also direct investments toward strengthening public health systems [9].
Your resilience plan should align with broader frameworks like National Adaptation Plans (NAPs) under the UN Framework Convention on Climate Change [9]. The World Health Organization highlights that resilience planning goes beyond infrastructure. It involves activities, partnerships, and the collective capacity of various actors within the health system [1]. Tailor specific indicators to track progress rather than relying on generic metrics, and integrate your efforts with existing health surveillance systems to avoid redundancy [1].
How Council Fire Supports Climate Resilience Planning
Expert guidance can turn even the most comprehensive plans into actionable strategies. Council Fire offers a systems-based approach to climate resilience planning, focusing on translating sustainability goals into measurable outcomes. Their expertise ensures organizations move beyond simple compliance, enabling them to create meaningful progress through data-driven insights and stakeholder-focused planning.
Council Fire’s services combine technical know-how with strategic communication, ensuring infrastructure is prepared for future challenges while addressing environmental, social, and economic goals. Their approach includes in-depth impact analysis, fostering trust through stakeholder engagement, and crafting communication strategies that inspire organizational change around sustainability.
Policy Development and Implementation
Incorporating climate considerations into health policies and daily operations is essential for creating resilient health systems. The WHO Operational Framework outlines 10 key components to guide this process [8][2]. By building on existing Hazard Vulnerability Analysis (HVA) processes, organizations can ensure climate resilience becomes a standard practice rather than an afterthought [5]. This approach forms a strong basis for integrating these considerations into cohesive health strategies.
Integrating Climate into Health Policies
Health policies should align with global frameworks such as National Adaptation Plans (NAPs), Universal Health Coverage, and the Sustainable Development Goals [8][2]. Infrastructure standards must also be updated to account for climate projections over the next 20–50 years, ensuring preparedness for future challenges [5]. Modern health systems must aim to be both climate-resilient and low-carbon [2].
"Failure to prepare for climate change now by bolstering the resilience of health systems increases the probability that hazards become disasters and complex emergencies that cause severe impacts to human health and communities."
WHO [1]
To ensure policies are practical and actionable, a multi-disciplinary team should be formed. This team might include representatives from Facilities, Security, Engineering, Nursing, Supply Chain, and Emergency Planning, ensuring that policies reflect operational realities [5].
Partnering Across Sectors
Health systems cannot achieve resilience in isolation. Collaboration with sectors such as energy, water, transportation, and emergency management is crucial to maintaining essential services during prolonged utility outages [5]. These sectors, often referred to as "health-determining sectors", play a direct role in ensuring care delivery during climate-related events [8][1]. For instance, formal Emergency Water Supply Plans should be developed to evaluate water usage, response capabilities, and alternative supply options like on-site wells or rainwater harvesting [5].
Beyond infrastructure, partnerships should include experts in nutrition and sanitation to address risks like food insecurity and waterborne diseases that are exacerbated by climate variability [8]. Once these cross-sector collaborations are in place, tracking progress becomes vital to ensuring effectiveness.
Tracking Progress and Results
"Measuring the climate resilience of a health system is most effectively done with information and indicators that are tailored to the needs of the health authority using it."
WHO [1]
To effectively measure progress, health systems should use indicators that address local health concerns rather than relying solely on broad international metrics [1]. Leveraging existing national health surveillance and monitoring infrastructure can help avoid redundancy [1]. It’s important to evaluate the system’s ability to anticipate, respond to, recover from, and adapt to climate-related challenges [1]. Tools such as the HHS ASPR Risk Identification and Site Criticality (RISC) Toolkit can provide baseline assessments, while the Climate Resilience for Health Care toolkit aids in integrating climate considerations into emergency preparedness plans [4].
Progress tracking should cover both health outcomes and the resilience of supporting infrastructure across various activities and actors within the health system [1]. Metrics should also include greenhouse gas emission reductions alongside resilience indicators to assess progress toward low-carbon operations [2]. For multi-campus health systems, site-specific assessments are essential, as risks and vulnerabilities can vary widely based on location and climate zone [5].
Conclusion and Key Takeaways
Building climate-resilient health systems is essential for safeguarding communities and ensuring uninterrupted care during extreme weather events. The strategies outlined here provide a structured approach for health organizations to address climate challenges while maintaining their ability to serve effectively.
Main Strategies Recap
Achieving climate resilience involves addressing both immediate vulnerabilities and long-term adaptation needs. Start with a detailed vulnerability assessment that combines climate projections with health data. From there, focus on creating resilient infrastructure by:
Assessing climate risks and considering future extremes in land use and building design.
Implementing sustainable energy and water solutions to protect critical systems.
Ensuring essential clinical services remain operational during disruptions.
Incorporating environmental protections like green infrastructure to mitigate risks.
As emphasized, integrating risk assessments with resilient design and fostering collaboration across sectors is vital for long-term success.
Collaboration with sectors such as energy, water, transportation, and emergency management is crucial for maintaining essential services during extended outages. Facilities that are less critical should aim to restore services within 48 to 96 hours after a major weather event [3].
To measure progress, use customized indicators that evaluate your system's capacity to anticipate, respond to, recover from, and adapt to climate-related challenges. These strategies offer a clear path for immediate and practical action.
Next Steps
Begin by conducting a standardized vulnerability assessment to identify weaknesses in infrastructure, communication systems, and supply chains. Instead of creating separate initiatives, integrate climate considerations into your existing emergency preparedness plans - resilience efforts are most effective when embedded into established processes.
Consider collaborating with experts who specialize in both sustainability and health system operations. For instance, Council Fire provides strategic guidance and actionable plans to help organizations build climate resilience. They focus on sustainable infrastructure, energy and water systems, and cross-sector partnerships, enabling health systems to balance environmental considerations with operational continuity. Their expertise can help accelerate progress toward a climate-resilient future while ensuring your health system remains dependable when your community needs it most.
FAQs
What makes a health system climate-resilient?
A climate-resilient health system is built to handle the growing challenges posed by climate change, such as extreme heat, floods, storms, and wildfires, while actively working to lower its own greenhouse gas (GHG) emissions. According to the World Health Organization, achieving this requires ten essential components, including effective governance, a skilled workforce, comprehensive climate risk assessments, and infrastructure designed with sustainability in mind.
These systems emphasize real-time monitoring, health programs tailored to climate realities, and strong emergency preparedness to safeguard communities from climate-related threats. Equally important are sustainable funding models and the use of advanced, climate-conscious technologies to ensure long-term resilience.
In the U.S., Council Fire supports health organizations in adopting these strategies. By providing expertise in areas like sustainable infrastructure, energy systems, and stakeholder collaboration, they help align climate initiatives with broader financial and social goals.
How can healthcare facilities identify and address climate-related risks effectively?
To tackle climate-related risks effectively, healthcare facilities must start by evaluating their unique vulnerabilities. This means collecting up-to-date, location-specific climate data to understand potential threats like floods, heat waves, wildfires, or rising sea levels. Facilities should then analyze how these risks could impact their infrastructure, utilities, and service areas. Tools like mapping software can be particularly useful for visualizing high-risk zones and pinpointing critical systems - such as power supplies or water infrastructure - that might be disrupted during extreme weather events.
After identifying these risks, prioritization is key. Facilities should rank threats based on their likelihood, the potential impact on essential services, and the specific needs of the community they serve. Practical steps might include installing backup generators, reinforcing building structures, and ensuring supply chains remain reliable under adverse conditions. Collaboration with stakeholders - such as staff, emergency managers, and local community members - can ensure solutions are both effective and tailored to the community's context.
Council Fire offers healthcare providers strategic support in assessing risks, planning, and implementing climate-resilient measures. By weaving these efforts into routine planning, healthcare systems can safeguard patient care while bolstering community resilience against climate-related challenges.
How do early warning systems help healthcare facilities prepare for extreme weather events?
Early warning systems are indispensable for keeping healthcare facilities operational during extreme weather events. By delivering timely alerts about potential threats like floods, heat waves, storms, or power outages, these systems enable hospitals, clinics, and long-term care facilities to take precautionary measures. Actions might include securing backup power sources, safeguarding critical medical equipment, pre-stocking necessary supplies, and organizing safe transportation for both staff and patients.
Incorporating early warning data into risk assessments allows healthcare organizations to better prepare for climate-related challenges over time. This approach strengthens both infrastructure and operations, ensuring greater resilience. Additionally, these systems facilitate the swift implementation of response protocols, such as activating shelter plans, establishing evacuation routes, and coordinating with community support networks. The result is minimized disruptions and enhanced safety for patients and healthcare workers alike.
Council Fire supports healthcare systems in integrating early warning capabilities into their emergency strategies, fostering coordinated efforts to maintain care delivery even during severe weather conditions.
Related Blog Posts

FAQ
01
What does it really mean to “redefine profit”?
02
What makes Council Fire different?
03
Who does Council Fire you work with?
04
What does working with Council Fire actually look like?
05
How does Council Fire help organizations turn big goals into action?
06
How does Council Fire define and measure success?


Dec 30, 2025
Guide to Climate-Resilient Health Systems
Capacity Building
In This Article
Health systems must assess climate risks, strengthen infrastructure, and use early warning and monitoring to keep medical services running during extreme weather.
Guide to Climate-Resilient Health Systems
The increasing frequency of extreme weather events like hurricanes, floods, and heat waves is putting healthcare systems under immense pressure. Climate-resilient health systems are designed to remain functional during such crises, ensuring uninterrupted medical services and support for communities. This guide outlines actionable steps, including conducting risk assessments, building robust infrastructure, and integrating early warning systems, to help healthcare facilities prepare for climate challenges.
Key Takeaways:
Risk Assessments: Identify threats using tools like the U.S. Climate Resilience Toolkit and WHO checklists.
Infrastructure Planning: Design facilities with future climate risks in mind, ensuring energy and water redundancy.
Surveillance and Monitoring: Use real-time systems to track and address climate-sensitive health risks.
Early Warning Systems: Develop protocols to maintain critical services during disruptions.
Collaboration: Work with local agencies, emergency teams, and community stakeholders for a coordinated response.
Start by mapping vulnerabilities, integrating climate and health data, and creating a resilience plan tailored to your facility’s needs. These strategies ensure healthcare systems can withstand and recover from climate-related disruptions while continuing to serve their communities effectively.
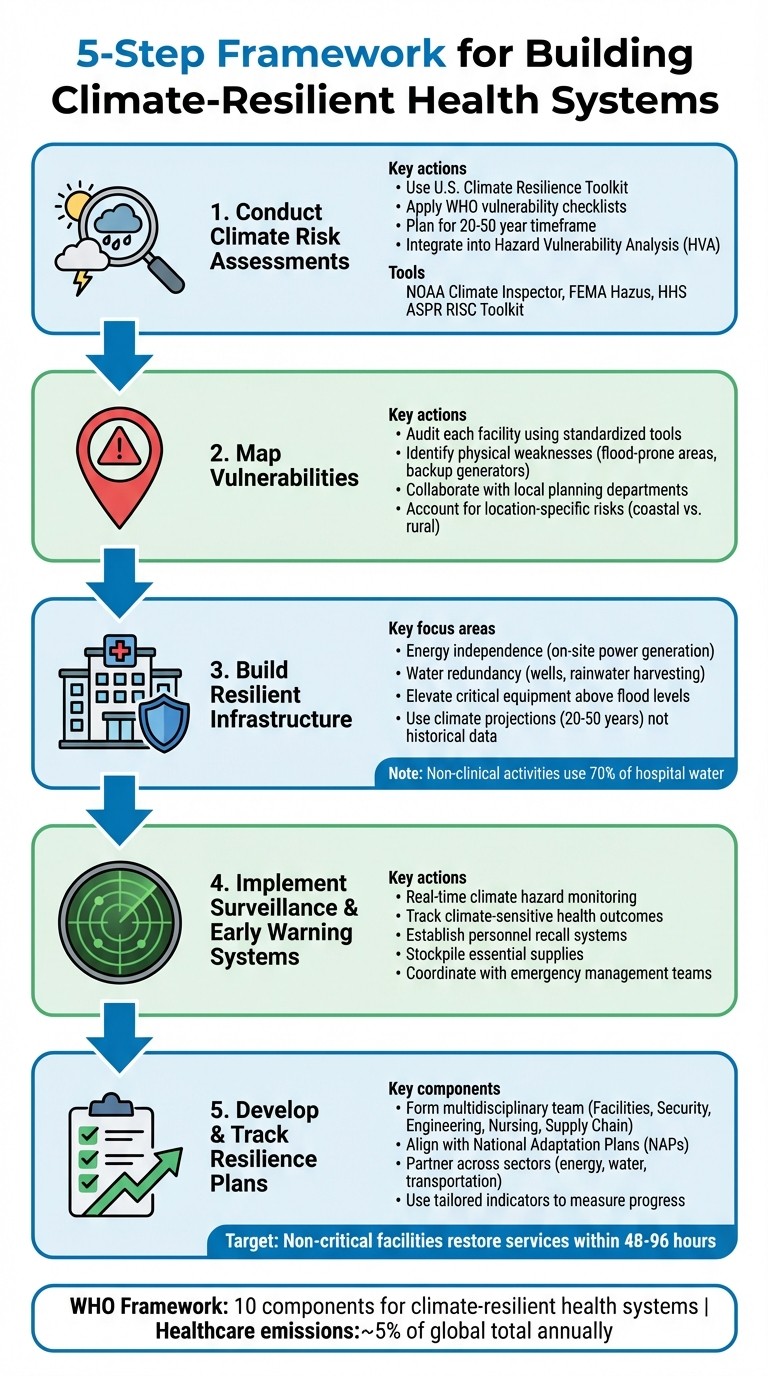
5-Step Framework for Building Climate-Resilient Health Systems
Building Climate-Resilient Health Systems
Conducting Climate Risk Assessments
To build resilience, healthcare systems first need to pinpoint potential threats through comprehensive climate risk assessments. These evaluations should account for both gradual changes, like rising sea levels, and sudden events, such as hurricanes or heat waves [6]. The U.S. Climate Resilience Toolkit highlights the importance of this process:
Health care organizations are encouraged to conduct a climate risk assessment so that they may better understand and catalog present and future extreme weather risks [6].
Such assessments are vital for long-term planning, typically spanning 20 to 50 years, and should be integrated into an organization's broader Hazard Vulnerability Analysis (HVA). This ensures a well-rounded, multi-hazard approach [6]. Once risks are identified, the next step is to map specific vulnerabilities at each facility to address these threats effectively.
How to Map Vulnerabilities
Mapping vulnerabilities requires a tailored approach, as risks vary significantly by location. For example, hospitals along Florida’s coast face threats like hurricanes and flooding, while facilities in rural Montana might contend with harsh winters or limited access to resources. Rural hospitals often serve as community hubs during emergencies, providing food, water, and shelter, whereas urban centers may focus on specialized medical care [6].
Begin by auditing each facility using standardized tools like the WHO "Checklists to Assess Vulnerabilities in Health Care Facilities" or the HHS "Climate Resilience Checklists." These tools help identify physical weaknesses, such as critical equipment located in flood-prone areas or backup generators that might fail under extreme heat [4][7]. Collaborate with local planning departments, municipal authorities, and community stakeholders to ensure your assessment aligns with regional climate projections [6]. If interpreting climate models proves challenging, consider partnering with local universities or sustainability consulting for expert guidance [6].
Combining Climate and Health Data
Once vulnerabilities are mapped, the next step is to integrate climate projections with health data. This combination provides a fuller picture of where impacts will hit hardest. Overlaying climate data with health statistics, disease prevalence, and socioeconomic factors helps identify populations most at risk [7]. The WHO underscores the value of this approach:
Vulnerability and Adaptation Assessments (V&As) are a key instrument to identify and prepare for changing health risks. V&A assessments can provide information for decision-makers on the extent and magnitude of likely health risks attributable to climate change [7].
This integration enables health systems to anticipate how climate shifts will influence disease patterns. For instance, rising temperatures could expand the range of mosquito-borne illnesses or accelerate pathogen incubation periods. By merging temperature projections with current disease surveillance, healthcare organizations can predict emerging health threats and allocate resources to areas of greatest need.
Predictive Tools and Frameworks
Several tools are available to simplify climate risk assessments. NOAA's Climate Inspector delivers localized projections for temperature and precipitation [6]. FEMA's Hazus software estimates potential losses from disasters like floods, hurricanes, and earthquakes [6]. The HHS ASPR RISC Toolkit (Risk Identification and Site Criticality) helps healthcare facilities identify risks and improve emergency preparedness [4]. For coastal areas, the Coastal Flood Exposure Mapper visualizes flooding risks, while CanVis offers photo-edited simulations of how sea-level rise could impact specific sites [6]. These tools allow healthcare systems to better prepare for and mitigate climate-driven disruptions.
These resources are part of larger frameworks, such as the WHO Operational Framework for Building Climate Resilient Health Systems. This framework includes 10 components, with risk assessment as a central element [7][8]. It also emphasizes the importance of addressing healthcare systems' own greenhouse gas emissions, which account for roughly 5% of global emissions annually [7]. By leveraging these tools and frameworks, healthcare organizations can take meaningful steps toward climate resilience.
Core Components of Climate-Resilient Health Systems
After identifying risks, healthcare organizations need to focus on the essential elements that ensure facilities remain functional during climate emergencies. These components work together to safeguard both infrastructure and patient care when extreme weather events occur.
Building Resilient Infrastructure
Strong infrastructure is the backbone of climate resilience. According to the U.S. Department of Health and Human Services:
Essential health services must remain available to communities and individuals during and immediately following extreme weather events, even during extended utility outages and transportation infrastructure disturbances. [5]
A major focus is energy independence. Facilities can boost resilience by adopting on-site power generation systems, such as Combined Heat and Power systems, which allow them to function even if the regional power grid fails. To further protect critical systems, fuel pumps, tanks, and electrical switchgear should be positioned above anticipated flood levels to reduce the risk of damage.
Water redundancy is another priority. On-site wells, rainwater harvesting systems, and reclaimed water solutions can ensure a steady supply. With non-clinical activities consuming up to 70% of hospital water [5], reclaimed systems can help maintain operations while easing the strain on municipal resources.
Infrastructure planning should also shift away from outdated historical data and instead rely on climate projections for the next 20 to 50 years. This forward-thinking approach can guide the design of roads, stormwater systems, and building structures to better withstand future conditions. Nature-based solutions, like advanced stormwater management and strategies to mitigate urban heat islands, can complement these efforts by supporting natural water flow and adding extra layers of protection.
Physical upgrades alone are not enough - real-time data and monitoring systems are essential for ensuring operational readiness.
Improving Surveillance and Monitoring
Real-time surveillance systems allow health facilities to anticipate and address climate-related risks before they escalate. Monitoring climate hazards and understanding community vulnerabilities not only aids immediate service delivery but also informs long-term planning. By tracking climate-sensitive health outcomes across different regions, these systems can pinpoint populations at the highest risk.
Advanced technologies can enhance these monitoring efforts. For example, integrating climate risk assessments into existing Hazard Vulnerability Analysis enables data-driven planning. This helps facilities prepare for patient surges and manage shelter-in-place scenarios for those with medical vulnerabilities.
Once robust surveillance systems are in place, they lay the groundwork for effective early warning responses.
Creating Early Warning and Response Systems
Early warning systems are crucial for activating response protocols that keep essential clinical services - such as emergency departments, imaging facilities, and laboratories - operational during and after extreme weather events. These systems rely on earlier risk assessments to trigger timely actions.
Effective response planning also hinges on clear personnel coordination. Facilities should establish recall systems in collaboration with local and regional emergency management teams to ensure medical and support staff can either reach the facility or remain on-site during transportation disruptions. Stockpiling essential supplies on-site further bolsters the ability to operate during extended disruptions to supply chains.
Early warning indicators, which can provide timelines ranging from weeks to years, give healthcare systems the ability to scale up capacity, secure backup resources, and work proactively with community partners to manage potential challenges.
Creating Climate Resilience Plans
Once vulnerabilities are mapped and resilient infrastructure is established, the next step is crafting a resilience plan. This plan brings previous risk assessments into action, ensuring uninterrupted services during climate-related events.
Planning Steps
Start with a Hazard Vulnerability Assessment (HVA) using tools like the RISC Toolkit to identify risks and critical facilities [4]. Build the plan around five key elements:
Updated Data: Incorporate the latest climate hazard and vulnerability information.
Resilient Design: Use land planning and building designs that anticipate future weather extremes.
Secured Systems: Establish energy, water, and waste systems designed to withstand extreme events throughout their entire lifespan [3].
Clinical Care Protocols: Develop procedures for maintaining essential care during patient surges, including sheltering in place when transportation is unavailable.
Environmental Measures: Implement green infrastructure and strategies to reduce heat islands across your campus [3].
For non-critical facilities, ensure plans allow for safe closures and quick service resumption within 48–96 hours [3].
Form a multidisciplinary team that includes members from Facilities, Security, Engineering, Nursing, Supply Chain, Emergency Planning, and other relevant departments. This ensures a thorough approach to planning [3]. Standardized tools, like the Sustainable and Climate-Resilient Health Care Facilities Toolkit, can help transform assessments into actionable strategies [3].
Working with Stakeholders
Use insights from your vulnerability maps to engage with local agencies and community leaders. Collaborate with emergency preparedness teams, public health officials, and other stakeholders - such as those in water, sanitation, and nutrition sectors - to address risks beyond your facility [9][4]. International development agencies can also direct investments toward strengthening public health systems [9].
Your resilience plan should align with broader frameworks like National Adaptation Plans (NAPs) under the UN Framework Convention on Climate Change [9]. The World Health Organization highlights that resilience planning goes beyond infrastructure. It involves activities, partnerships, and the collective capacity of various actors within the health system [1]. Tailor specific indicators to track progress rather than relying on generic metrics, and integrate your efforts with existing health surveillance systems to avoid redundancy [1].
How Council Fire Supports Climate Resilience Planning
Expert guidance can turn even the most comprehensive plans into actionable strategies. Council Fire offers a systems-based approach to climate resilience planning, focusing on translating sustainability goals into measurable outcomes. Their expertise ensures organizations move beyond simple compliance, enabling them to create meaningful progress through data-driven insights and stakeholder-focused planning.
Council Fire’s services combine technical know-how with strategic communication, ensuring infrastructure is prepared for future challenges while addressing environmental, social, and economic goals. Their approach includes in-depth impact analysis, fostering trust through stakeholder engagement, and crafting communication strategies that inspire organizational change around sustainability.
Policy Development and Implementation
Incorporating climate considerations into health policies and daily operations is essential for creating resilient health systems. The WHO Operational Framework outlines 10 key components to guide this process [8][2]. By building on existing Hazard Vulnerability Analysis (HVA) processes, organizations can ensure climate resilience becomes a standard practice rather than an afterthought [5]. This approach forms a strong basis for integrating these considerations into cohesive health strategies.
Integrating Climate into Health Policies
Health policies should align with global frameworks such as National Adaptation Plans (NAPs), Universal Health Coverage, and the Sustainable Development Goals [8][2]. Infrastructure standards must also be updated to account for climate projections over the next 20–50 years, ensuring preparedness for future challenges [5]. Modern health systems must aim to be both climate-resilient and low-carbon [2].
"Failure to prepare for climate change now by bolstering the resilience of health systems increases the probability that hazards become disasters and complex emergencies that cause severe impacts to human health and communities."
WHO [1]
To ensure policies are practical and actionable, a multi-disciplinary team should be formed. This team might include representatives from Facilities, Security, Engineering, Nursing, Supply Chain, and Emergency Planning, ensuring that policies reflect operational realities [5].
Partnering Across Sectors
Health systems cannot achieve resilience in isolation. Collaboration with sectors such as energy, water, transportation, and emergency management is crucial to maintaining essential services during prolonged utility outages [5]. These sectors, often referred to as "health-determining sectors", play a direct role in ensuring care delivery during climate-related events [8][1]. For instance, formal Emergency Water Supply Plans should be developed to evaluate water usage, response capabilities, and alternative supply options like on-site wells or rainwater harvesting [5].
Beyond infrastructure, partnerships should include experts in nutrition and sanitation to address risks like food insecurity and waterborne diseases that are exacerbated by climate variability [8]. Once these cross-sector collaborations are in place, tracking progress becomes vital to ensuring effectiveness.
Tracking Progress and Results
"Measuring the climate resilience of a health system is most effectively done with information and indicators that are tailored to the needs of the health authority using it."
WHO [1]
To effectively measure progress, health systems should use indicators that address local health concerns rather than relying solely on broad international metrics [1]. Leveraging existing national health surveillance and monitoring infrastructure can help avoid redundancy [1]. It’s important to evaluate the system’s ability to anticipate, respond to, recover from, and adapt to climate-related challenges [1]. Tools such as the HHS ASPR Risk Identification and Site Criticality (RISC) Toolkit can provide baseline assessments, while the Climate Resilience for Health Care toolkit aids in integrating climate considerations into emergency preparedness plans [4].
Progress tracking should cover both health outcomes and the resilience of supporting infrastructure across various activities and actors within the health system [1]. Metrics should also include greenhouse gas emission reductions alongside resilience indicators to assess progress toward low-carbon operations [2]. For multi-campus health systems, site-specific assessments are essential, as risks and vulnerabilities can vary widely based on location and climate zone [5].
Conclusion and Key Takeaways
Building climate-resilient health systems is essential for safeguarding communities and ensuring uninterrupted care during extreme weather events. The strategies outlined here provide a structured approach for health organizations to address climate challenges while maintaining their ability to serve effectively.
Main Strategies Recap
Achieving climate resilience involves addressing both immediate vulnerabilities and long-term adaptation needs. Start with a detailed vulnerability assessment that combines climate projections with health data. From there, focus on creating resilient infrastructure by:
Assessing climate risks and considering future extremes in land use and building design.
Implementing sustainable energy and water solutions to protect critical systems.
Ensuring essential clinical services remain operational during disruptions.
Incorporating environmental protections like green infrastructure to mitigate risks.
As emphasized, integrating risk assessments with resilient design and fostering collaboration across sectors is vital for long-term success.
Collaboration with sectors such as energy, water, transportation, and emergency management is crucial for maintaining essential services during extended outages. Facilities that are less critical should aim to restore services within 48 to 96 hours after a major weather event [3].
To measure progress, use customized indicators that evaluate your system's capacity to anticipate, respond to, recover from, and adapt to climate-related challenges. These strategies offer a clear path for immediate and practical action.
Next Steps
Begin by conducting a standardized vulnerability assessment to identify weaknesses in infrastructure, communication systems, and supply chains. Instead of creating separate initiatives, integrate climate considerations into your existing emergency preparedness plans - resilience efforts are most effective when embedded into established processes.
Consider collaborating with experts who specialize in both sustainability and health system operations. For instance, Council Fire provides strategic guidance and actionable plans to help organizations build climate resilience. They focus on sustainable infrastructure, energy and water systems, and cross-sector partnerships, enabling health systems to balance environmental considerations with operational continuity. Their expertise can help accelerate progress toward a climate-resilient future while ensuring your health system remains dependable when your community needs it most.
FAQs
What makes a health system climate-resilient?
A climate-resilient health system is built to handle the growing challenges posed by climate change, such as extreme heat, floods, storms, and wildfires, while actively working to lower its own greenhouse gas (GHG) emissions. According to the World Health Organization, achieving this requires ten essential components, including effective governance, a skilled workforce, comprehensive climate risk assessments, and infrastructure designed with sustainability in mind.
These systems emphasize real-time monitoring, health programs tailored to climate realities, and strong emergency preparedness to safeguard communities from climate-related threats. Equally important are sustainable funding models and the use of advanced, climate-conscious technologies to ensure long-term resilience.
In the U.S., Council Fire supports health organizations in adopting these strategies. By providing expertise in areas like sustainable infrastructure, energy systems, and stakeholder collaboration, they help align climate initiatives with broader financial and social goals.
How can healthcare facilities identify and address climate-related risks effectively?
To tackle climate-related risks effectively, healthcare facilities must start by evaluating their unique vulnerabilities. This means collecting up-to-date, location-specific climate data to understand potential threats like floods, heat waves, wildfires, or rising sea levels. Facilities should then analyze how these risks could impact their infrastructure, utilities, and service areas. Tools like mapping software can be particularly useful for visualizing high-risk zones and pinpointing critical systems - such as power supplies or water infrastructure - that might be disrupted during extreme weather events.
After identifying these risks, prioritization is key. Facilities should rank threats based on their likelihood, the potential impact on essential services, and the specific needs of the community they serve. Practical steps might include installing backup generators, reinforcing building structures, and ensuring supply chains remain reliable under adverse conditions. Collaboration with stakeholders - such as staff, emergency managers, and local community members - can ensure solutions are both effective and tailored to the community's context.
Council Fire offers healthcare providers strategic support in assessing risks, planning, and implementing climate-resilient measures. By weaving these efforts into routine planning, healthcare systems can safeguard patient care while bolstering community resilience against climate-related challenges.
How do early warning systems help healthcare facilities prepare for extreme weather events?
Early warning systems are indispensable for keeping healthcare facilities operational during extreme weather events. By delivering timely alerts about potential threats like floods, heat waves, storms, or power outages, these systems enable hospitals, clinics, and long-term care facilities to take precautionary measures. Actions might include securing backup power sources, safeguarding critical medical equipment, pre-stocking necessary supplies, and organizing safe transportation for both staff and patients.
Incorporating early warning data into risk assessments allows healthcare organizations to better prepare for climate-related challenges over time. This approach strengthens both infrastructure and operations, ensuring greater resilience. Additionally, these systems facilitate the swift implementation of response protocols, such as activating shelter plans, establishing evacuation routes, and coordinating with community support networks. The result is minimized disruptions and enhanced safety for patients and healthcare workers alike.
Council Fire supports healthcare systems in integrating early warning capabilities into their emergency strategies, fostering coordinated efforts to maintain care delivery even during severe weather conditions.
Related Blog Posts

FAQ
What does it really mean to “redefine profit”?
What makes Council Fire different?
Who does Council Fire you work with?
What does working with Council Fire actually look like?
How does Council Fire help organizations turn big goals into action?
How does Council Fire define and measure success?


