


Dec 21, 2025
Dec 21, 2025
How to Benchmark Healthcare Sustainability Goals
Sustainability Strategy
Sustainability Strategy
In This Article
Guide to benchmarking healthcare sustainability: set SMART goals, measure energy, water, waste and emissions, and use governance and tools to save costs.
How to Benchmark Healthcare Sustainability Goals
Healthcare organizations face increasing pressure to meet environmental targets while controlling costs and improving patient care. Benchmarking sustainability goals provides a clear path to measure, compare, and improve performance. By analyzing resource use, emissions, and waste management, hospitals can identify inefficiencies, reduce costs, and align with stakeholder expectations. In 2023 alone, U.S. hospitals saved over $182 million through such initiatives, conserving energy, water, and reducing landfill waste.
Key Takeaways:
Why Benchmarking Matters: Tracks progress, identifies inefficiencies, and ensures compliance with regulations.
SMART Goals: Set specific, measurable, achievable, relevant, and time-bound targets (e.g., reducing hazardous waste by 20% by 2026).
Metrics to Measure: Focus on energy (kBtu/sq. ft.), water (gallons/sq. ft.), waste diversion rates, and greenhouse gas reductions.
Tools and Resources: Use platforms like Practice Greenhealth reports and ASHE dashboards to normalize data and set benchmarks.
Governance: Establish a "Green Team" with a sustainability champion reporting to executive leadership.
By integrating sustainability into core operations, healthcare organizations can achieve measurable results that benefit both their mission and the planet.
A greener pharmaceutical supply chain for the people and planet


Aligning Sustainability Goals with Organizational Priorities
Sustainability plays a critical role in healthcare, as environmental factors directly influence conditions like asthma, cancer, and heat-related illnesses. By prioritizing sustainability, healthcare organizations not only protect the environment but also strengthen their clinical mission.
Setting Up Sustainability Governance
Establishing an effective governance structure is key to success. Start by appointing a Sustainability Champion who reports directly to executive leadership. This individual will lead a multidisciplinary "Green Team" or steering committee, which should include an executive sponsor from the C-suite, the CFO, operational leaders from facilities and supply chain, and clinical leaders capable of driving practice changes [4].
"Hospital and health systems engaged in sustainable practices are doing so largely because it aligns with their humanitarian and stewardship mission and vision." - ASHE [6]
For larger organizations, consider a multi-tiered approach. A central council can oversee broad strategies, while sub-committees focus on specific areas like energy, waste management, or clinical practices [4]. To ensure consistency, develop a shared sustainability glossary so all departments use the same language when discussing goals and metrics [4][6].
Once governance is in place, the next step is to define clear and measurable sustainability targets.
Creating SMART Sustainability Goals
Sustainability goals should follow the SMART framework: Specific, Measurable, Achievable, Relevant, and Time-bound. For instance, you might aim to cut red bag waste by 20% by December 31, 2026, which would also lead to notable cost savings [4].
Implement a Measurement and Verification (M&V) protocol early to track progress transparently and provide data-backed results to stakeholders like the CFO [4]. Begin with low-risk initiatives that deliver immediate results without affecting clinical care. For example, energy efficiency upgrades often yield quick savings. Conduct waste audits to identify items mistakenly placed in red bag waste that could be recycled or disposed of as general waste [4]. Additionally, collaborate with anesthesiologists to transition away from high-global warming potential gases, such as nitrous oxide, to alternatives like isoflurane [4].
These well-defined goals create a solid foundation for aligning sustainability efforts with both financial and clinical objectives.
Connecting Sustainability to Value-Based Care
Linking sustainability initiatives to value-based care can drive long-term health outcomes while reducing costs. Energy efficiency and waste reduction not only lower operational expenses but also contribute to healthier environments, enhancing patient care.
One effective strategy is to establish a "Climate Fund." Savings from low-cost interventions, such as automated HVAC adjustments or staff behavior changes, can be reinvested into high-impact sustainability projects [7]. Since fossil fuel emissions account for approximately 95% of a hospital's Scope 1 and 2 emissions, focusing on energy reduction offers a direct route to both decarbonization and cost savings [4]. This approach shows leadership and stakeholders that sustainability investments deliver measurable returns while advancing the organization’s mission of care and stewardship.
Selecting and Measuring Healthcare Sustainability Metrics
Healthcare Sustainability Benchmarking: Key Metrics and Performance Indicators
Once governance structures and goals are in place, the next step is to identify metrics that accurately measure progress. Having precise measurements transforms sustainability aspirations into tangible actions. As Elizabeth Schenk, PhD, RN, Chief Environmental Stewardship Officer at Providence, emphasizes:
"Educated guesses just don't have the same power as real numbers when it comes to driving change" [8].
These metrics serve as the foundation for evaluating sustainability efforts in a structured and meaningful way.
Key Performance Indicators (KPIs) for Healthcare
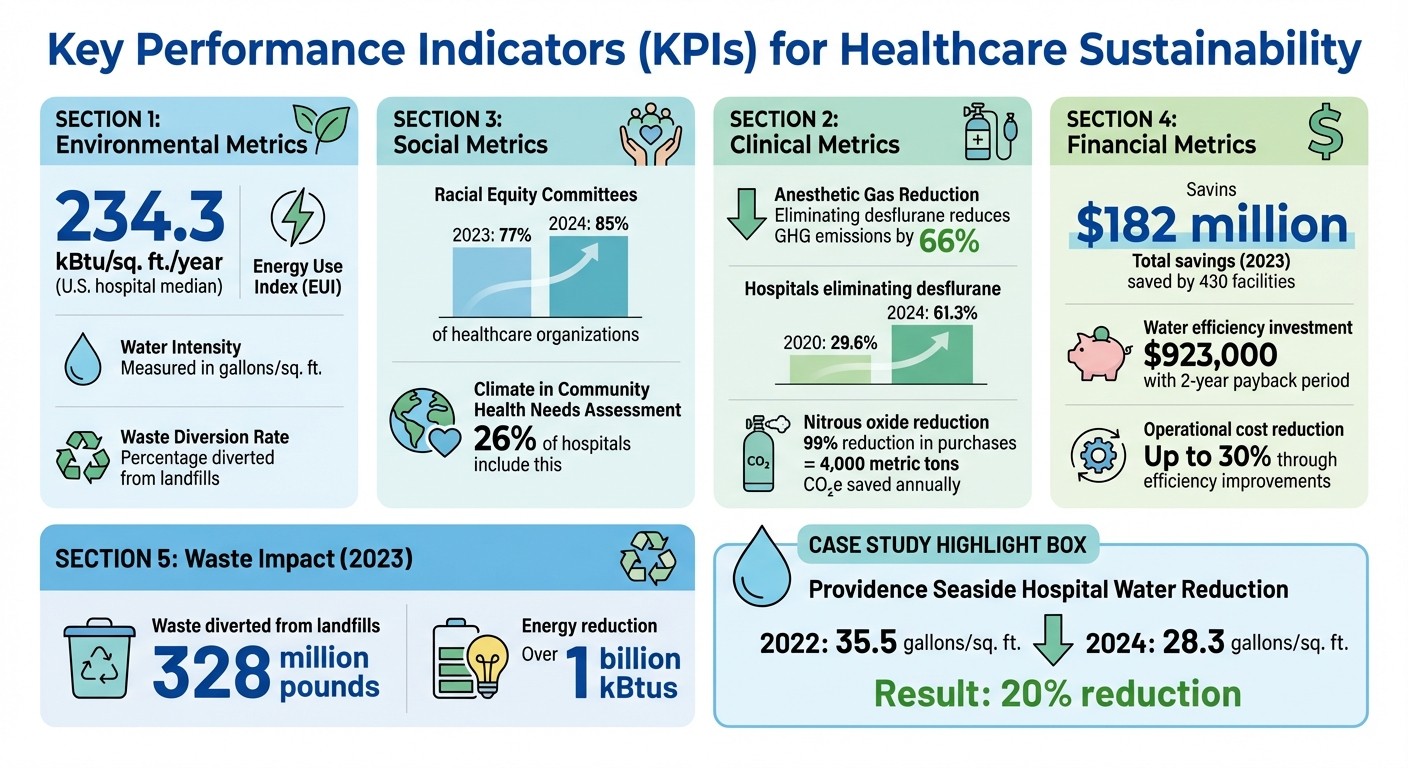
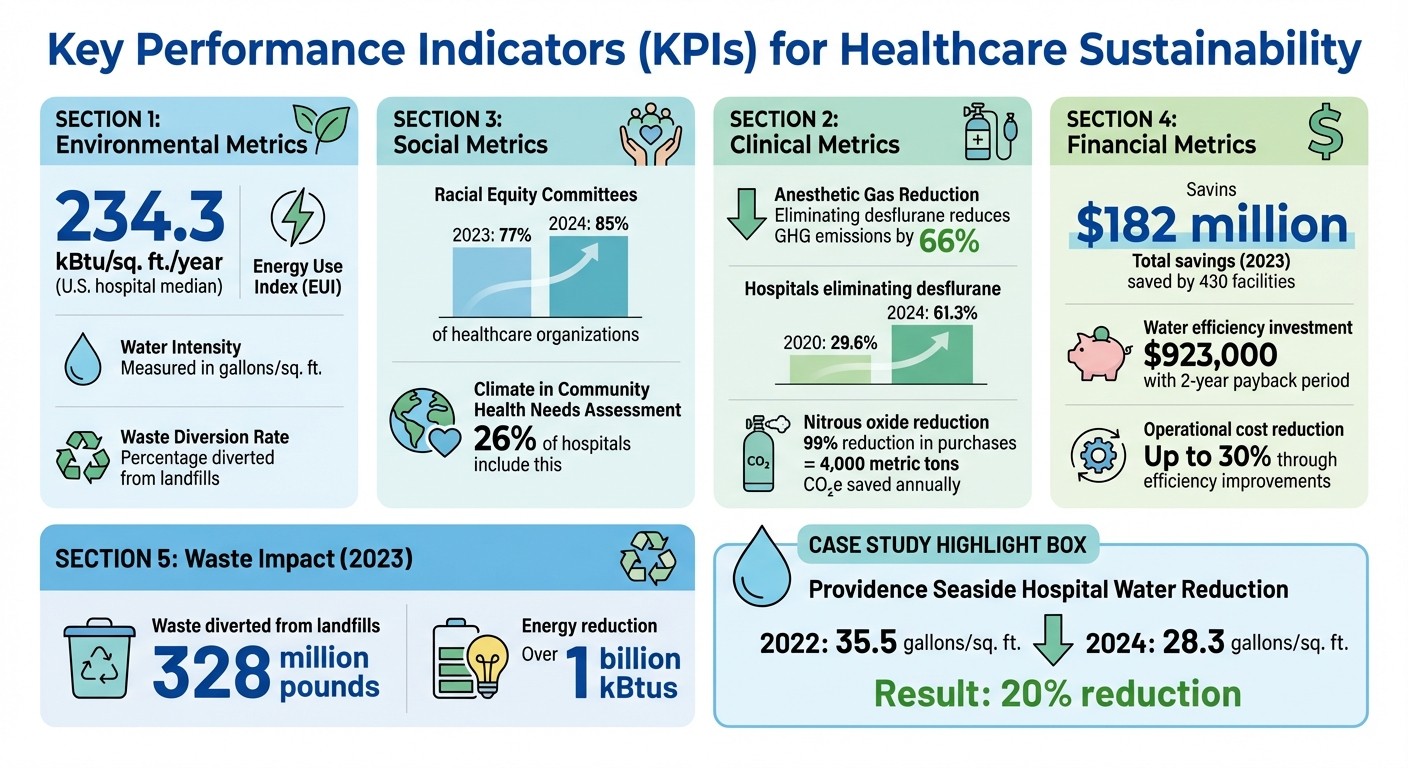
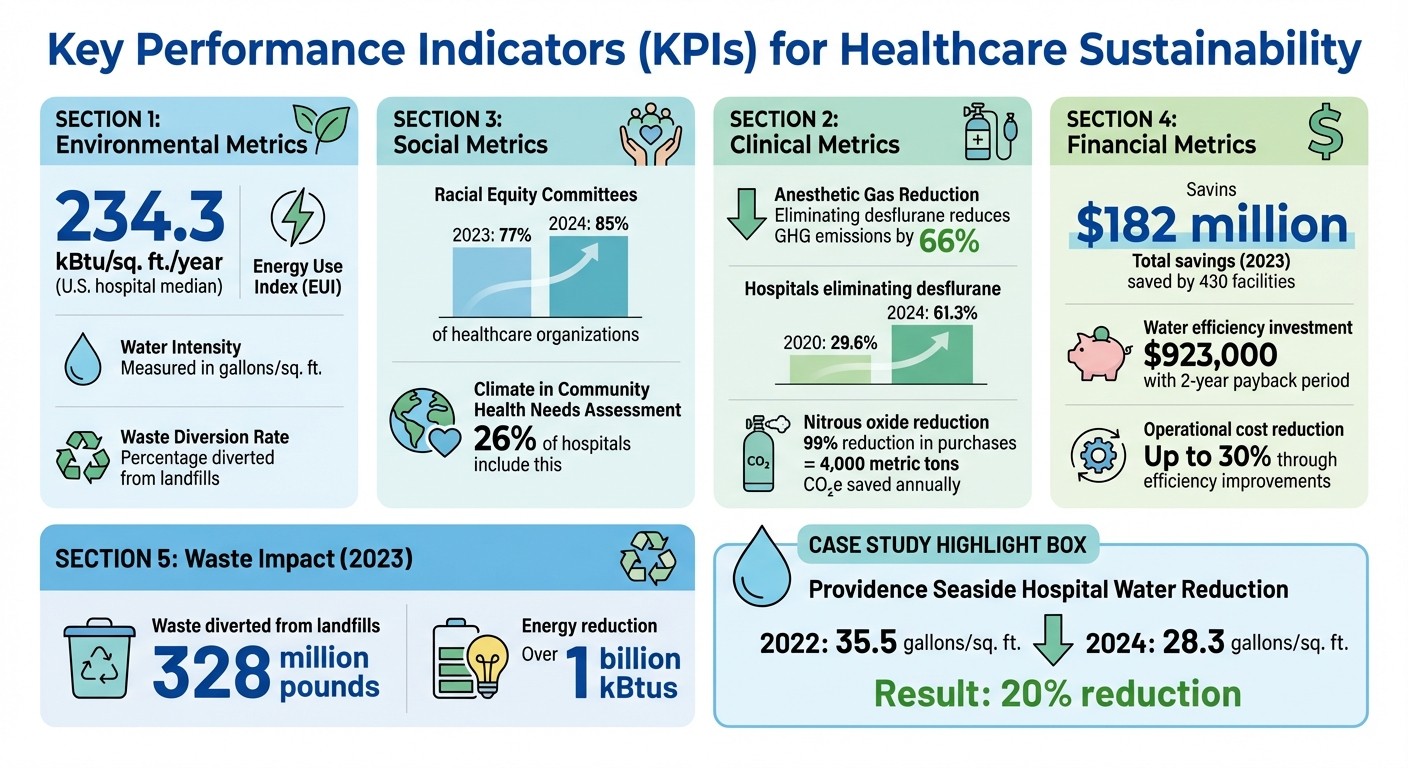
Healthcare organizations should focus on metrics across four key areas: environmental, clinical, social, and financial. For environmental performance, metrics like the Energy Use Index (EUI) - measured in kBtu per square foot annually - are critical. The national median for U.S. hospitals is 234.3 kBtu/sq. ft./year [8]. Other environmental indicators include water intensity (gallons per square foot) and waste diversion rates, which track the percentage of waste diverted from landfills.
Clinical metrics often target high-impact areas such as anesthetic gases. For instance, eliminating the use of desflurane can lower greenhouse gas emissions by 66% [5]. Social metrics focus on equity initiatives, with 85% of healthcare applicants in 2024 reporting the formation of internal racial equity committees, compared to 77% in 2023 [5]. Financial KPIs capture savings from sustainability projects, such as reduced landfill fees and returns on investments in efficiency improvements.
Metric Category | Key Performance Indicator (KPI) | Common Units |
|---|---|---|
Energy | Energy Use Index (EUI) | kBtu/sq. ft./year |
Water | Water Intensity | Gallons/sq. ft. |
Waste | Waste Optimization Score | % Diverted from Landfill |
Clinical | Anesthetic Gas Reduction | Metric tons CO₂e |
Social | Racial Equity Governance | % of facilities with committees |
Financial | Sustainability Savings | USD ($) |
Data Sources and Normalization Methods
After selecting metrics, the next challenge is gathering accurate data and ensuring fair comparisons. Data can be sourced from utility bills, waste invoices, electronic health records (EHRs), and supplier reports. However, raw numbers alone are insufficient. To provide meaningful insights, data should be standardized - whether by square footage, patient days, or full-time equivalent staff [8].
For example, Providence Seaside Hospital reduced its water consumption from 35.5 gallons per square foot in 2022 to 28.3 gallons per square foot by mid-2024, thanks to targeted facility upgrades led by Andy Mason, the hospital's facilities director [8]. This normalized metric allowed the leadership to compare performance across its 51-hospital network, leading to a $923,000 investment in water efficiency projects with an anticipated two-year payback period [8].
When integrating new data sources, allow two quarters for validation [8]. Additionally, push vendors to provide auditable electronic data rather than estimates. Geoffrey Glass, Senior Manager for Energy and Sustainability at Providence, explains:
"Within a minute you can tell what you're doing well and where you have opportunities to improve. We now benchmark using validated data" [8].
Equity and Risk-Adjusted Metrics
Not all healthcare facilities operate under the same conditions. Differences in patient populations, climate, and infrastructure mean that equity-sensitive and risk-adjusted metrics are essential. For example, hospitals with EUI scores below 150 often deliver lower-intensity care, while those exceeding 300 may operate in extreme climates or rely on outdated infrastructure [8].
Metrics should also account for patient complexity and social determinants of health. A hospital serving a high-acuity population will naturally consume more resources than an outpatient clinic. Between 2017 and 2020, Dr. Brian Chesebro at Providence discovered that while clinical use of nitrous oxide dropped by 61%, emissions from purchases remained high due to undetected leaks in central supply lines [8]. By comparing purchase data with EHR usage, the team identified discrepancies, switched to portable tanks at 17 hospitals, and reduced nitrous oxide purchases by 99%, cutting 4,000 metric tons of CO₂e annually [8]. This approach highlights how risk-adjusted analysis can uncover inefficiencies that traditional metrics might overlook, enabling organizations to set more realistic and impactful goals.
Benchmarking Against Internal and External Standards
Accurate metrics allow organizations to measure their performance and compare it against both internal benchmarks and industry standards, uncovering their current position and areas for growth.
Internal vs External Benchmarking
Internal benchmarking focuses on tracking progress within an organization over time or comparing performance across different facilities in a system [9][11]. This method is particularly useful for real-time evaluations of past and present performance, helping refine goals and direct resources effectively [3]. For instance, in a multi-site system, you might identify which locations excel in water conservation or waste reduction and replicate those successful practices across other sites.
External benchmarking, on the other hand, involves comparing your organization’s performance against peer institutions and national standards to identify gaps and opportunities [3][11]. This approach helps you stay informed about industry trends, assess the return on investment of strategies used by others, and adopt proven best practices [11]. By turning raw data into actionable insights, external benchmarking provides a broader perspective on where your organization stands.
Most organizations use a combination of both methods. Internal benchmarking ensures site-specific improvements and better resource management, while external benchmarking offers valuable context for how your performance measures up within the industry [3][11]. Together, these insights help guide the selection of effective benchmarking tools to achieve sustainability goals.
Using External Benchmarking Tools
Once key metrics are established, external benchmarking tools can validate and challenge your internal targets. One widely used tool in U.S. healthcare is the Practice Greenhealth Sustainability Benchmark Report, which allows hospitals to compare their performance with over 1,500 peer facilities [3][11]. Member hospitals receive annual report cards that benchmark their performance across 30 metrics [12]. These metrics span 11 impact areas, including leadership, waste, chemicals, operating room practices, food, energy, water, and climate [10][1].
Such benchmarks not only highlight potential savings and resource efficiencies but also provide early insights into Scope 3 emissions - those related to supply chain impacts. This data offers one of the first comprehensive glimpses into this critical area within the healthcare sector [5].
Organizations rely on these tools to conduct gap analyses, pinpointing areas where they fall behind industry medians or top-performing institutions [12]. Notably, 89% of respondents in 2023 reported having a sustainability leader at the health system level, and 62% of hospitals now report sustainability progress directly to their board of directors [13].
Applying Benchmarks to Set Targets
External benchmarks can also serve as a foundation for setting actionable and measurable targets. For example, using 90th percentile benchmarks enables organizations to establish ambitious long-term goals [12]. This data is also instrumental in securing investments from leadership. For instance, showing that eliminating desflurane led to a 66% reduction in greenhouse gas emissions provides a compelling argument for similar initiatives [5].
To maximize the impact of benchmarking, align these insights with broader organizational goals. This could mean linking sustainability objectives to value-based care models, community health needs assessments, or racial equity initiatives. For example, 26% of hospitals now include climate change considerations in their Community Health Needs Assessment process, while 85% have established internal racial equity committees - an increase from 77% in 2023 [5][13]. These connections ensure that sustainability efforts contribute meaningfully to the organization’s overall mission.
Turning Insights Into Action
Benchmarking data becomes truly valuable when it drives clear and prioritized actions that seamlessly integrate into existing systems. Below, we explore how to transform these insights into meaningful, actionable targets.
Setting Realistic and Ambitious Targets
Sustainability targets should strike a balance between ambition and practicality. Benchmarking data can guide the establishment of short-term achievements while laying the foundation for long-term transformational goals. For instance, if a facility's energy efficiency currently falls in the mid-range, a short-term goal might involve significant performance improvements within a year, paired with a longer-term aim to achieve near-top efficiency.
Focus on key resource areas - energy, water, waste, and materials - where the data reveals the most significant opportunities [3]. Break these targets into specific categories. For example, phasing out desflurane, a high-impact anesthetic gas, can dramatically reduce greenhouse gas emissions. Between 2020 and 2024, the percentage of hospitals eliminating desflurane nearly doubled, rising from 29.6% to 61.3%, underscoring how bold goals can inspire industry-wide progress [5]. In waste management, set diversion rate targets. In 2023, participating facilities successfully diverted over 328 million pounds of waste from landfills through recycling programs [5].
Prioritizing Initiatives by Impact
Once realistic targets are defined, prioritize initiatives that deliver the highest returns. Consider factors like financial impact, feasibility, and alignment with clinical priorities [6].
Organize efforts into four major areas: Transportation, Buildings & Energy Use, Anesthetic Gases, and Waste [2]. Within each category, address the largest contributors first. For example, fossil fuel emissions typically account for 95% of a hospital's Scope 1 and 2 emissions, making energy efficiency upgrades a logical starting point [4].
Engage multidisciplinary teams to identify quick, high-impact wins, such as fixing nitrous oxide leaks or upgrading lighting systems [4][6]. Conduct waste audits to uncover cost-saving opportunities. For example, reducing red bag waste can slash disposal costs significantly, as regulated medical waste is far more expensive to handle than general waste [4]. Similarly, addressing nitrous oxide tank leaks and switching to lower-impact anesthetic agents like isoflurane can effectively cut greenhouse gas emissions while controlling costs [4].
Adding Sustainability to Performance Management
Embedding sustainability metrics into daily performance management ensures continuous progress toward established goals. To drive accountability, sustainability goals should be integrated into existing performance systems. Appoint a sustainability champion with a clear reporting line to facility managers or department heads, supported by an executive sponsor from the C-suite [4]. This dual governance structure ensures both operational effectiveness and strategic alignment.
Create multidisciplinary green teams with clearly assigned tasks and regular, structured meetings [4]. In 2024, 85% of healthcare organizations reported forming internal committees focused on racial equity, up from 77% in 2023, demonstrating how formal structures can enhance accountability [5].
Implement a measurement and verification (M&V) protocol early to track savings and monitor progress [4]. This protocol should be adaptable to accommodate renovations or expansions. Digital tools, like the Energy to Care Dashboard, provide real-time energy performance tracking and help communicate progress toward sustainability goals [4][6].
Incorporate sustainability KPIs into executive scorecards and operational dashboards. Steven Rice, CHRO of The Bill & Melinda Gates Foundation, emphasizes the importance of actionable data:
"I believe that the data will set you free. At the end of the day, it's about how you turn those pieces of information into insights that will improve business" [3].
Align sustainability metrics with capital planning cycles, setting both short-term and long-term goals for energy, water, and waste reduction [4]. Use internal communication channels, such as newsletters, to share measurable energy savings and highlight staff contributions [4]. Publicizing achievements fosters momentum and reinforces the message that sustainability is a central organizational priority. When sustainability metrics are tracked alongside clinical quality and financial performance indicators, it reinforces that environmental stewardship is an integral part of the organization's mission [6].
Maintaining Continuous Improvement and Resilience
Sustainability benchmarking isn’t a one-and-done task; it’s an ongoing process that adjusts to new challenges, regulations, and opportunities. By embedding resilience into your sustainability efforts, you can better navigate both gradual changes and sudden disruptions.
Annual Benchmarking Cycles
Conducting an annual review helps maintain a clear, adaptable foundation for your sustainability goals. Structured reporting cycles, such as the Practice Greenhealth Environmental Excellence Awards, provide a framework to document progress and account for changes like facility renovations or equipment updates. Early implementation of a Measurement and Verification (M&V) protocol, alongside tools like the ASHE Energy to Care Dashboard, allows for real-time tracking and strategic adjustments [3][4][5].
The results speak volumes: in 2023, nearly 430 healthcare facilities participating in these cycles collectively saved over $182 million, reduced energy use by more than 1 billion kBtus, and diverted 328 million pounds of waste from landfills [5]. These reviews also help assess the effectiveness of targeted interventions. For instance, hospitals phasing out desflurane nearly doubled their progress from 29.6% in 2020 to 61.3% in 2024, cutting associated greenhouse gas emissions by 66% [5].
Beyond these scheduled reviews, preparing for unexpected events through scenario planning is essential to maintaining operational resilience.
Scenario Planning for Climate Resilience
With climate disruptions on the rise, scenario planning has become critical for safeguarding healthcare operations. This requires a multidisciplinary approach, bringing together teams from Facilities, Nursing, Supply Chain, Engineering, Sustainability, and Emergency Planning. These groups can integrate climate resilience into existing emergency preparedness and hazard vulnerability analyses (HVA) [15].
Reassess infrastructure capabilities to account for extreme weather events that exceed historical norms. For example, resilience plans should consider "black-start" and "islanding" capabilities, ensuring that critical services remain powered even during prolonged grid outages. On-site solar power paired with battery storage can provide a reliable energy source when both the grid and backup generators fail [17].
Tools like the HHS Administration for Strategic Preparedness and Response (ASPR) Risk Identification and Site Criticality (RISC) Toolkit can support forward-looking risk assessments [16]. Resilience planning should focus on key areas such as climate risk data, infrastructure protection, land use, clinical care continuity, and environmental safeguards [15]. Collaborating with community partners and government agencies ensures compliance with state-specific mandates, such as Washington State's Clean Buildings Law or New York's Climate Leadership and Community Protection Act [15][17].
As your resilience strategies evolve, so too should the metrics you use to measure progress.
Updating Metrics and Methods
Sustainability priorities shift over time, and your metrics need to keep pace. For instance, in 2024, 85% of healthcare organizations reported forming internal committees focused on racial equity - up from 77% in 2023 - showing how sustainability now encompasses social impact alongside environmental goals [5].
Expand your metrics to include Scope 3 emissions estimates and clinical waste data. In 2023, 49 facilities successfully eliminated harmful chemicals like PVC and DEHP from at least two medical product categories within two years [5]. Metrics should also account for potent greenhouse gases, such as refrigerants and nitrous oxide, which have significant global warming potential [4].
Real-time data analysis is essential for making informed decisions quickly [3]. Adding qualitative insights to your benchmarking data - such as explanations of performance trends, areas of high resource use, or planned efficiency projects - can provide valuable context. This narrative approach helps stakeholders see the bigger picture and builds support for future initiatives [14].
At Council Fire (https://councilfire.org), we emphasize an integrated strategy - combining regular benchmarking, proactive scenario planning, and evolving metrics to create lasting sustainability in healthcare.
Conclusion
Achieving sustainability in healthcare demands a well-structured approach, combining clear governance, aligned objectives, and a commitment to continuous improvement. The numbers speak for themselves: organizations that adopt comprehensive sustainability practices can cut operational costs by as much as 30% through enhanced efficiency and waste reduction [3].
The role of an engaged workforce cannot be overstated. Success hinges on staff who not only understand the goals but also receive proper training and see tangible results. Formal green teams - comprising members from both executive leadership and frontline staff - can unify efforts toward shared sustainability objectives.
The importance of setting SMART goals and conducting regular benchmarking is highlighted by the Joint Commission, which emphasizes accountability and strategic alignment [2]. These practices form the backbone of a cyclical process, encompassing goal-setting and continuous refinement.
Sustainability is a dynamic endeavor. Metrics and methodologies must adapt to emerging challenges, leveraging tools like real-time data analytics to make swift, informed decisions. This flexibility ensures strategies remain relevant and capitalize on new opportunities as they arise.
"I believe that the data will set you free. At the end of the day, it's about how you turn those pieces of information into insights that will improve business" [3].
Steven Rice, CHRO at The Bill & Melinda Gates Foundation
FAQs
How can healthcare organizations track and measure their sustainability goals effectively?
To effectively measure progress in sustainability, healthcare organizations should begin by gathering baseline data. This involves assessing direct emissions (Scope 1), indirect emissions from energy usage (Scope 2), and broader supply chain impacts (Scope 3), as categorized by the Greenhouse Gas Protocol. Conducting facility assessments, energy and waste audits, and supply chain inventories can provide the necessary information. Converting measurements such as kilowatt-hours, gallons, or cubic feet into CO₂e equivalents allows for meaningful year-over-year comparisons.
Once the baseline is established, organizations can measure their performance against industry benchmarks, like those found in Practice Greenhealth’s annual Sustainability Benchmark Report. Regular updates to dashboards with real-time or monthly data - covering metrics like energy savings, water use reduction, or waste management - enable organizations to turn raw numbers into actionable insights. Tools such as the ENERGY STAR® Portfolio Manager can simplify the process of tracking and reporting.
Council Fire offers strategic support to healthcare organizations in areas like data collection, fostering collaboration among stakeholders, and communicating progress. By leveraging standardized methods and benchmarking tools, hospitals can achieve tangible results, such as cutting CO₂e emissions by 15% or saving $1.2 million annually, all while contributing to national climate objectives.
What challenges do healthcare organizations face when setting SMART sustainability goals?
Healthcare organizations face a range of obstacles when attempting to establish SMART (Specific, Measurable, Achievable, Relevant, Time-bound) sustainability goals. A primary issue is the absence of reliable baseline data. Many facilities find it challenging to accurately track direct emissions (Scope 1) and indirect emissions from purchased energy (Scope 2). Tackling Scope 3 emissions - such as those from supply chain operations, waste management, and employee commuting - proves even more difficult. Without dependable data, creating measurable and verifiable goals becomes a daunting task.
Another significant hurdle is the lack of consistent industry benchmarks. While some organizations report notable savings, individual facilities often lack a standardized way to evaluate their performance against similar institutions. This gap makes it harder to set targets that are both realistic and ambitious. Adding to the complexity, fragmented reporting standards across the industry further hinder progress.
Lastly, gaining alignment among diverse stakeholders poses a challenge. Clinicians, facility managers, procurement teams, and leadership often have differing priorities, and internal silos can obstruct collaboration. Successful sustainability strategies demand teamwork, transparency, and unified goals, yet competing agendas frequently slow momentum. Overcoming these barriers is essential for achieving impactful sustainability results.
How can healthcare facilities align sustainability goals with value-based care models?
Healthcare facilities can weave sustainability goals into value-based care (VBC) models by incorporating environmental performance into their assessments of quality and cost. By monitoring data such as energy usage, waste production, water consumption, and supply chain emissions alongside clinical outcomes and expenses, hospitals can measure the financial and environmental benefits of eco-friendly initiatives. For instance, efforts like reducing utility bills or cutting waste disposal costs can directly contribute to both cost savings and improved care quality.
Collaboration plays a crucial role in making this integration effective. Engaging clinicians, payers, and patients in setting benchmarks allows facilities to align sustainability goals with reimbursement incentives. For example, cutting back on carbon-heavy practices - such as minimizing energy-intensive equipment use or addressing emissions from supply chains - can lead to better care at lower costs. Transparent reporting of these outcomes helps build trust and enables payers to reward facilities that achieve both clinical and environmental objectives.
Working with sustainability-focused organizations like Council Fire provides healthcare systems with the tools and strategies needed to balance financial goals with environmental and social progress. These partnerships bring the expertise required to embed sustainable practices into performance metrics, fostering ongoing improvements in both healthcare delivery and environmental stewardship.
Related Blog Posts

Latest Articles
©2025
FAQ
FAQ
01
What does it really mean to “redefine profit”?
02
What makes Council Fire different?
03
Who does Council Fire you work with?
04
What does working with Council Fire actually look like?
05
How does Council Fire help organizations turn big goals into action?
06
How does Council Fire define and measure success?
01
What does it really mean to “redefine profit”?
02
What makes Council Fire different?
03
Who does Council Fire you work with?
04
What does working with Council Fire actually look like?
05
How does Council Fire help organizations turn big goals into action?
06
How does Council Fire define and measure success?


Dec 21, 2025
How to Benchmark Healthcare Sustainability Goals
Sustainability Strategy
In This Article
Guide to benchmarking healthcare sustainability: set SMART goals, measure energy, water, waste and emissions, and use governance and tools to save costs.
How to Benchmark Healthcare Sustainability Goals
Healthcare organizations face increasing pressure to meet environmental targets while controlling costs and improving patient care. Benchmarking sustainability goals provides a clear path to measure, compare, and improve performance. By analyzing resource use, emissions, and waste management, hospitals can identify inefficiencies, reduce costs, and align with stakeholder expectations. In 2023 alone, U.S. hospitals saved over $182 million through such initiatives, conserving energy, water, and reducing landfill waste.
Key Takeaways:
Why Benchmarking Matters: Tracks progress, identifies inefficiencies, and ensures compliance with regulations.
SMART Goals: Set specific, measurable, achievable, relevant, and time-bound targets (e.g., reducing hazardous waste by 20% by 2026).
Metrics to Measure: Focus on energy (kBtu/sq. ft.), water (gallons/sq. ft.), waste diversion rates, and greenhouse gas reductions.
Tools and Resources: Use platforms like Practice Greenhealth reports and ASHE dashboards to normalize data and set benchmarks.
Governance: Establish a "Green Team" with a sustainability champion reporting to executive leadership.
By integrating sustainability into core operations, healthcare organizations can achieve measurable results that benefit both their mission and the planet.
A greener pharmaceutical supply chain for the people and planet

Aligning Sustainability Goals with Organizational Priorities
Sustainability plays a critical role in healthcare, as environmental factors directly influence conditions like asthma, cancer, and heat-related illnesses. By prioritizing sustainability, healthcare organizations not only protect the environment but also strengthen their clinical mission.
Setting Up Sustainability Governance
Establishing an effective governance structure is key to success. Start by appointing a Sustainability Champion who reports directly to executive leadership. This individual will lead a multidisciplinary "Green Team" or steering committee, which should include an executive sponsor from the C-suite, the CFO, operational leaders from facilities and supply chain, and clinical leaders capable of driving practice changes [4].
"Hospital and health systems engaged in sustainable practices are doing so largely because it aligns with their humanitarian and stewardship mission and vision." - ASHE [6]
For larger organizations, consider a multi-tiered approach. A central council can oversee broad strategies, while sub-committees focus on specific areas like energy, waste management, or clinical practices [4]. To ensure consistency, develop a shared sustainability glossary so all departments use the same language when discussing goals and metrics [4][6].
Once governance is in place, the next step is to define clear and measurable sustainability targets.
Creating SMART Sustainability Goals
Sustainability goals should follow the SMART framework: Specific, Measurable, Achievable, Relevant, and Time-bound. For instance, you might aim to cut red bag waste by 20% by December 31, 2026, which would also lead to notable cost savings [4].
Implement a Measurement and Verification (M&V) protocol early to track progress transparently and provide data-backed results to stakeholders like the CFO [4]. Begin with low-risk initiatives that deliver immediate results without affecting clinical care. For example, energy efficiency upgrades often yield quick savings. Conduct waste audits to identify items mistakenly placed in red bag waste that could be recycled or disposed of as general waste [4]. Additionally, collaborate with anesthesiologists to transition away from high-global warming potential gases, such as nitrous oxide, to alternatives like isoflurane [4].
These well-defined goals create a solid foundation for aligning sustainability efforts with both financial and clinical objectives.
Connecting Sustainability to Value-Based Care
Linking sustainability initiatives to value-based care can drive long-term health outcomes while reducing costs. Energy efficiency and waste reduction not only lower operational expenses but also contribute to healthier environments, enhancing patient care.
One effective strategy is to establish a "Climate Fund." Savings from low-cost interventions, such as automated HVAC adjustments or staff behavior changes, can be reinvested into high-impact sustainability projects [7]. Since fossil fuel emissions account for approximately 95% of a hospital's Scope 1 and 2 emissions, focusing on energy reduction offers a direct route to both decarbonization and cost savings [4]. This approach shows leadership and stakeholders that sustainability investments deliver measurable returns while advancing the organization’s mission of care and stewardship.
Selecting and Measuring Healthcare Sustainability Metrics
Healthcare Sustainability Benchmarking: Key Metrics and Performance Indicators
Once governance structures and goals are in place, the next step is to identify metrics that accurately measure progress. Having precise measurements transforms sustainability aspirations into tangible actions. As Elizabeth Schenk, PhD, RN, Chief Environmental Stewardship Officer at Providence, emphasizes:
"Educated guesses just don't have the same power as real numbers when it comes to driving change" [8].
These metrics serve as the foundation for evaluating sustainability efforts in a structured and meaningful way.
Key Performance Indicators (KPIs) for Healthcare
Healthcare organizations should focus on metrics across four key areas: environmental, clinical, social, and financial. For environmental performance, metrics like the Energy Use Index (EUI) - measured in kBtu per square foot annually - are critical. The national median for U.S. hospitals is 234.3 kBtu/sq. ft./year [8]. Other environmental indicators include water intensity (gallons per square foot) and waste diversion rates, which track the percentage of waste diverted from landfills.
Clinical metrics often target high-impact areas such as anesthetic gases. For instance, eliminating the use of desflurane can lower greenhouse gas emissions by 66% [5]. Social metrics focus on equity initiatives, with 85% of healthcare applicants in 2024 reporting the formation of internal racial equity committees, compared to 77% in 2023 [5]. Financial KPIs capture savings from sustainability projects, such as reduced landfill fees and returns on investments in efficiency improvements.
Metric Category | Key Performance Indicator (KPI) | Common Units |
|---|---|---|
Energy | Energy Use Index (EUI) | kBtu/sq. ft./year |
Water | Water Intensity | Gallons/sq. ft. |
Waste | Waste Optimization Score | % Diverted from Landfill |
Clinical | Anesthetic Gas Reduction | Metric tons CO₂e |
Social | Racial Equity Governance | % of facilities with committees |
Financial | Sustainability Savings | USD ($) |
Data Sources and Normalization Methods
After selecting metrics, the next challenge is gathering accurate data and ensuring fair comparisons. Data can be sourced from utility bills, waste invoices, electronic health records (EHRs), and supplier reports. However, raw numbers alone are insufficient. To provide meaningful insights, data should be standardized - whether by square footage, patient days, or full-time equivalent staff [8].
For example, Providence Seaside Hospital reduced its water consumption from 35.5 gallons per square foot in 2022 to 28.3 gallons per square foot by mid-2024, thanks to targeted facility upgrades led by Andy Mason, the hospital's facilities director [8]. This normalized metric allowed the leadership to compare performance across its 51-hospital network, leading to a $923,000 investment in water efficiency projects with an anticipated two-year payback period [8].
When integrating new data sources, allow two quarters for validation [8]. Additionally, push vendors to provide auditable electronic data rather than estimates. Geoffrey Glass, Senior Manager for Energy and Sustainability at Providence, explains:
"Within a minute you can tell what you're doing well and where you have opportunities to improve. We now benchmark using validated data" [8].
Equity and Risk-Adjusted Metrics
Not all healthcare facilities operate under the same conditions. Differences in patient populations, climate, and infrastructure mean that equity-sensitive and risk-adjusted metrics are essential. For example, hospitals with EUI scores below 150 often deliver lower-intensity care, while those exceeding 300 may operate in extreme climates or rely on outdated infrastructure [8].
Metrics should also account for patient complexity and social determinants of health. A hospital serving a high-acuity population will naturally consume more resources than an outpatient clinic. Between 2017 and 2020, Dr. Brian Chesebro at Providence discovered that while clinical use of nitrous oxide dropped by 61%, emissions from purchases remained high due to undetected leaks in central supply lines [8]. By comparing purchase data with EHR usage, the team identified discrepancies, switched to portable tanks at 17 hospitals, and reduced nitrous oxide purchases by 99%, cutting 4,000 metric tons of CO₂e annually [8]. This approach highlights how risk-adjusted analysis can uncover inefficiencies that traditional metrics might overlook, enabling organizations to set more realistic and impactful goals.
Benchmarking Against Internal and External Standards
Accurate metrics allow organizations to measure their performance and compare it against both internal benchmarks and industry standards, uncovering their current position and areas for growth.
Internal vs External Benchmarking
Internal benchmarking focuses on tracking progress within an organization over time or comparing performance across different facilities in a system [9][11]. This method is particularly useful for real-time evaluations of past and present performance, helping refine goals and direct resources effectively [3]. For instance, in a multi-site system, you might identify which locations excel in water conservation or waste reduction and replicate those successful practices across other sites.
External benchmarking, on the other hand, involves comparing your organization’s performance against peer institutions and national standards to identify gaps and opportunities [3][11]. This approach helps you stay informed about industry trends, assess the return on investment of strategies used by others, and adopt proven best practices [11]. By turning raw data into actionable insights, external benchmarking provides a broader perspective on where your organization stands.
Most organizations use a combination of both methods. Internal benchmarking ensures site-specific improvements and better resource management, while external benchmarking offers valuable context for how your performance measures up within the industry [3][11]. Together, these insights help guide the selection of effective benchmarking tools to achieve sustainability goals.
Using External Benchmarking Tools
Once key metrics are established, external benchmarking tools can validate and challenge your internal targets. One widely used tool in U.S. healthcare is the Practice Greenhealth Sustainability Benchmark Report, which allows hospitals to compare their performance with over 1,500 peer facilities [3][11]. Member hospitals receive annual report cards that benchmark their performance across 30 metrics [12]. These metrics span 11 impact areas, including leadership, waste, chemicals, operating room practices, food, energy, water, and climate [10][1].
Such benchmarks not only highlight potential savings and resource efficiencies but also provide early insights into Scope 3 emissions - those related to supply chain impacts. This data offers one of the first comprehensive glimpses into this critical area within the healthcare sector [5].
Organizations rely on these tools to conduct gap analyses, pinpointing areas where they fall behind industry medians or top-performing institutions [12]. Notably, 89% of respondents in 2023 reported having a sustainability leader at the health system level, and 62% of hospitals now report sustainability progress directly to their board of directors [13].
Applying Benchmarks to Set Targets
External benchmarks can also serve as a foundation for setting actionable and measurable targets. For example, using 90th percentile benchmarks enables organizations to establish ambitious long-term goals [12]. This data is also instrumental in securing investments from leadership. For instance, showing that eliminating desflurane led to a 66% reduction in greenhouse gas emissions provides a compelling argument for similar initiatives [5].
To maximize the impact of benchmarking, align these insights with broader organizational goals. This could mean linking sustainability objectives to value-based care models, community health needs assessments, or racial equity initiatives. For example, 26% of hospitals now include climate change considerations in their Community Health Needs Assessment process, while 85% have established internal racial equity committees - an increase from 77% in 2023 [5][13]. These connections ensure that sustainability efforts contribute meaningfully to the organization’s overall mission.
Turning Insights Into Action
Benchmarking data becomes truly valuable when it drives clear and prioritized actions that seamlessly integrate into existing systems. Below, we explore how to transform these insights into meaningful, actionable targets.
Setting Realistic and Ambitious Targets
Sustainability targets should strike a balance between ambition and practicality. Benchmarking data can guide the establishment of short-term achievements while laying the foundation for long-term transformational goals. For instance, if a facility's energy efficiency currently falls in the mid-range, a short-term goal might involve significant performance improvements within a year, paired with a longer-term aim to achieve near-top efficiency.
Focus on key resource areas - energy, water, waste, and materials - where the data reveals the most significant opportunities [3]. Break these targets into specific categories. For example, phasing out desflurane, a high-impact anesthetic gas, can dramatically reduce greenhouse gas emissions. Between 2020 and 2024, the percentage of hospitals eliminating desflurane nearly doubled, rising from 29.6% to 61.3%, underscoring how bold goals can inspire industry-wide progress [5]. In waste management, set diversion rate targets. In 2023, participating facilities successfully diverted over 328 million pounds of waste from landfills through recycling programs [5].
Prioritizing Initiatives by Impact
Once realistic targets are defined, prioritize initiatives that deliver the highest returns. Consider factors like financial impact, feasibility, and alignment with clinical priorities [6].
Organize efforts into four major areas: Transportation, Buildings & Energy Use, Anesthetic Gases, and Waste [2]. Within each category, address the largest contributors first. For example, fossil fuel emissions typically account for 95% of a hospital's Scope 1 and 2 emissions, making energy efficiency upgrades a logical starting point [4].
Engage multidisciplinary teams to identify quick, high-impact wins, such as fixing nitrous oxide leaks or upgrading lighting systems [4][6]. Conduct waste audits to uncover cost-saving opportunities. For example, reducing red bag waste can slash disposal costs significantly, as regulated medical waste is far more expensive to handle than general waste [4]. Similarly, addressing nitrous oxide tank leaks and switching to lower-impact anesthetic agents like isoflurane can effectively cut greenhouse gas emissions while controlling costs [4].
Adding Sustainability to Performance Management
Embedding sustainability metrics into daily performance management ensures continuous progress toward established goals. To drive accountability, sustainability goals should be integrated into existing performance systems. Appoint a sustainability champion with a clear reporting line to facility managers or department heads, supported by an executive sponsor from the C-suite [4]. This dual governance structure ensures both operational effectiveness and strategic alignment.
Create multidisciplinary green teams with clearly assigned tasks and regular, structured meetings [4]. In 2024, 85% of healthcare organizations reported forming internal committees focused on racial equity, up from 77% in 2023, demonstrating how formal structures can enhance accountability [5].
Implement a measurement and verification (M&V) protocol early to track savings and monitor progress [4]. This protocol should be adaptable to accommodate renovations or expansions. Digital tools, like the Energy to Care Dashboard, provide real-time energy performance tracking and help communicate progress toward sustainability goals [4][6].
Incorporate sustainability KPIs into executive scorecards and operational dashboards. Steven Rice, CHRO of The Bill & Melinda Gates Foundation, emphasizes the importance of actionable data:
"I believe that the data will set you free. At the end of the day, it's about how you turn those pieces of information into insights that will improve business" [3].
Align sustainability metrics with capital planning cycles, setting both short-term and long-term goals for energy, water, and waste reduction [4]. Use internal communication channels, such as newsletters, to share measurable energy savings and highlight staff contributions [4]. Publicizing achievements fosters momentum and reinforces the message that sustainability is a central organizational priority. When sustainability metrics are tracked alongside clinical quality and financial performance indicators, it reinforces that environmental stewardship is an integral part of the organization's mission [6].
Maintaining Continuous Improvement and Resilience
Sustainability benchmarking isn’t a one-and-done task; it’s an ongoing process that adjusts to new challenges, regulations, and opportunities. By embedding resilience into your sustainability efforts, you can better navigate both gradual changes and sudden disruptions.
Annual Benchmarking Cycles
Conducting an annual review helps maintain a clear, adaptable foundation for your sustainability goals. Structured reporting cycles, such as the Practice Greenhealth Environmental Excellence Awards, provide a framework to document progress and account for changes like facility renovations or equipment updates. Early implementation of a Measurement and Verification (M&V) protocol, alongside tools like the ASHE Energy to Care Dashboard, allows for real-time tracking and strategic adjustments [3][4][5].
The results speak volumes: in 2023, nearly 430 healthcare facilities participating in these cycles collectively saved over $182 million, reduced energy use by more than 1 billion kBtus, and diverted 328 million pounds of waste from landfills [5]. These reviews also help assess the effectiveness of targeted interventions. For instance, hospitals phasing out desflurane nearly doubled their progress from 29.6% in 2020 to 61.3% in 2024, cutting associated greenhouse gas emissions by 66% [5].
Beyond these scheduled reviews, preparing for unexpected events through scenario planning is essential to maintaining operational resilience.
Scenario Planning for Climate Resilience
With climate disruptions on the rise, scenario planning has become critical for safeguarding healthcare operations. This requires a multidisciplinary approach, bringing together teams from Facilities, Nursing, Supply Chain, Engineering, Sustainability, and Emergency Planning. These groups can integrate climate resilience into existing emergency preparedness and hazard vulnerability analyses (HVA) [15].
Reassess infrastructure capabilities to account for extreme weather events that exceed historical norms. For example, resilience plans should consider "black-start" and "islanding" capabilities, ensuring that critical services remain powered even during prolonged grid outages. On-site solar power paired with battery storage can provide a reliable energy source when both the grid and backup generators fail [17].
Tools like the HHS Administration for Strategic Preparedness and Response (ASPR) Risk Identification and Site Criticality (RISC) Toolkit can support forward-looking risk assessments [16]. Resilience planning should focus on key areas such as climate risk data, infrastructure protection, land use, clinical care continuity, and environmental safeguards [15]. Collaborating with community partners and government agencies ensures compliance with state-specific mandates, such as Washington State's Clean Buildings Law or New York's Climate Leadership and Community Protection Act [15][17].
As your resilience strategies evolve, so too should the metrics you use to measure progress.
Updating Metrics and Methods
Sustainability priorities shift over time, and your metrics need to keep pace. For instance, in 2024, 85% of healthcare organizations reported forming internal committees focused on racial equity - up from 77% in 2023 - showing how sustainability now encompasses social impact alongside environmental goals [5].
Expand your metrics to include Scope 3 emissions estimates and clinical waste data. In 2023, 49 facilities successfully eliminated harmful chemicals like PVC and DEHP from at least two medical product categories within two years [5]. Metrics should also account for potent greenhouse gases, such as refrigerants and nitrous oxide, which have significant global warming potential [4].
Real-time data analysis is essential for making informed decisions quickly [3]. Adding qualitative insights to your benchmarking data - such as explanations of performance trends, areas of high resource use, or planned efficiency projects - can provide valuable context. This narrative approach helps stakeholders see the bigger picture and builds support for future initiatives [14].
At Council Fire (https://councilfire.org), we emphasize an integrated strategy - combining regular benchmarking, proactive scenario planning, and evolving metrics to create lasting sustainability in healthcare.
Conclusion
Achieving sustainability in healthcare demands a well-structured approach, combining clear governance, aligned objectives, and a commitment to continuous improvement. The numbers speak for themselves: organizations that adopt comprehensive sustainability practices can cut operational costs by as much as 30% through enhanced efficiency and waste reduction [3].
The role of an engaged workforce cannot be overstated. Success hinges on staff who not only understand the goals but also receive proper training and see tangible results. Formal green teams - comprising members from both executive leadership and frontline staff - can unify efforts toward shared sustainability objectives.
The importance of setting SMART goals and conducting regular benchmarking is highlighted by the Joint Commission, which emphasizes accountability and strategic alignment [2]. These practices form the backbone of a cyclical process, encompassing goal-setting and continuous refinement.
Sustainability is a dynamic endeavor. Metrics and methodologies must adapt to emerging challenges, leveraging tools like real-time data analytics to make swift, informed decisions. This flexibility ensures strategies remain relevant and capitalize on new opportunities as they arise.
"I believe that the data will set you free. At the end of the day, it's about how you turn those pieces of information into insights that will improve business" [3].
Steven Rice, CHRO at The Bill & Melinda Gates Foundation
FAQs
How can healthcare organizations track and measure their sustainability goals effectively?
To effectively measure progress in sustainability, healthcare organizations should begin by gathering baseline data. This involves assessing direct emissions (Scope 1), indirect emissions from energy usage (Scope 2), and broader supply chain impacts (Scope 3), as categorized by the Greenhouse Gas Protocol. Conducting facility assessments, energy and waste audits, and supply chain inventories can provide the necessary information. Converting measurements such as kilowatt-hours, gallons, or cubic feet into CO₂e equivalents allows for meaningful year-over-year comparisons.
Once the baseline is established, organizations can measure their performance against industry benchmarks, like those found in Practice Greenhealth’s annual Sustainability Benchmark Report. Regular updates to dashboards with real-time or monthly data - covering metrics like energy savings, water use reduction, or waste management - enable organizations to turn raw numbers into actionable insights. Tools such as the ENERGY STAR® Portfolio Manager can simplify the process of tracking and reporting.
Council Fire offers strategic support to healthcare organizations in areas like data collection, fostering collaboration among stakeholders, and communicating progress. By leveraging standardized methods and benchmarking tools, hospitals can achieve tangible results, such as cutting CO₂e emissions by 15% or saving $1.2 million annually, all while contributing to national climate objectives.
What challenges do healthcare organizations face when setting SMART sustainability goals?
Healthcare organizations face a range of obstacles when attempting to establish SMART (Specific, Measurable, Achievable, Relevant, Time-bound) sustainability goals. A primary issue is the absence of reliable baseline data. Many facilities find it challenging to accurately track direct emissions (Scope 1) and indirect emissions from purchased energy (Scope 2). Tackling Scope 3 emissions - such as those from supply chain operations, waste management, and employee commuting - proves even more difficult. Without dependable data, creating measurable and verifiable goals becomes a daunting task.
Another significant hurdle is the lack of consistent industry benchmarks. While some organizations report notable savings, individual facilities often lack a standardized way to evaluate their performance against similar institutions. This gap makes it harder to set targets that are both realistic and ambitious. Adding to the complexity, fragmented reporting standards across the industry further hinder progress.
Lastly, gaining alignment among diverse stakeholders poses a challenge. Clinicians, facility managers, procurement teams, and leadership often have differing priorities, and internal silos can obstruct collaboration. Successful sustainability strategies demand teamwork, transparency, and unified goals, yet competing agendas frequently slow momentum. Overcoming these barriers is essential for achieving impactful sustainability results.
How can healthcare facilities align sustainability goals with value-based care models?
Healthcare facilities can weave sustainability goals into value-based care (VBC) models by incorporating environmental performance into their assessments of quality and cost. By monitoring data such as energy usage, waste production, water consumption, and supply chain emissions alongside clinical outcomes and expenses, hospitals can measure the financial and environmental benefits of eco-friendly initiatives. For instance, efforts like reducing utility bills or cutting waste disposal costs can directly contribute to both cost savings and improved care quality.
Collaboration plays a crucial role in making this integration effective. Engaging clinicians, payers, and patients in setting benchmarks allows facilities to align sustainability goals with reimbursement incentives. For example, cutting back on carbon-heavy practices - such as minimizing energy-intensive equipment use or addressing emissions from supply chains - can lead to better care at lower costs. Transparent reporting of these outcomes helps build trust and enables payers to reward facilities that achieve both clinical and environmental objectives.
Working with sustainability-focused organizations like Council Fire provides healthcare systems with the tools and strategies needed to balance financial goals with environmental and social progress. These partnerships bring the expertise required to embed sustainable practices into performance metrics, fostering ongoing improvements in both healthcare delivery and environmental stewardship.
Related Blog Posts

FAQ
01
What does it really mean to “redefine profit”?
02
What makes Council Fire different?
03
Who does Council Fire you work with?
04
What does working with Council Fire actually look like?
05
How does Council Fire help organizations turn big goals into action?
06
How does Council Fire define and measure success?


Dec 21, 2025
How to Benchmark Healthcare Sustainability Goals
Sustainability Strategy
In This Article
Guide to benchmarking healthcare sustainability: set SMART goals, measure energy, water, waste and emissions, and use governance and tools to save costs.
How to Benchmark Healthcare Sustainability Goals
Healthcare organizations face increasing pressure to meet environmental targets while controlling costs and improving patient care. Benchmarking sustainability goals provides a clear path to measure, compare, and improve performance. By analyzing resource use, emissions, and waste management, hospitals can identify inefficiencies, reduce costs, and align with stakeholder expectations. In 2023 alone, U.S. hospitals saved over $182 million through such initiatives, conserving energy, water, and reducing landfill waste.
Key Takeaways:
Why Benchmarking Matters: Tracks progress, identifies inefficiencies, and ensures compliance with regulations.
SMART Goals: Set specific, measurable, achievable, relevant, and time-bound targets (e.g., reducing hazardous waste by 20% by 2026).
Metrics to Measure: Focus on energy (kBtu/sq. ft.), water (gallons/sq. ft.), waste diversion rates, and greenhouse gas reductions.
Tools and Resources: Use platforms like Practice Greenhealth reports and ASHE dashboards to normalize data and set benchmarks.
Governance: Establish a "Green Team" with a sustainability champion reporting to executive leadership.
By integrating sustainability into core operations, healthcare organizations can achieve measurable results that benefit both their mission and the planet.
A greener pharmaceutical supply chain for the people and planet

Aligning Sustainability Goals with Organizational Priorities
Sustainability plays a critical role in healthcare, as environmental factors directly influence conditions like asthma, cancer, and heat-related illnesses. By prioritizing sustainability, healthcare organizations not only protect the environment but also strengthen their clinical mission.
Setting Up Sustainability Governance
Establishing an effective governance structure is key to success. Start by appointing a Sustainability Champion who reports directly to executive leadership. This individual will lead a multidisciplinary "Green Team" or steering committee, which should include an executive sponsor from the C-suite, the CFO, operational leaders from facilities and supply chain, and clinical leaders capable of driving practice changes [4].
"Hospital and health systems engaged in sustainable practices are doing so largely because it aligns with their humanitarian and stewardship mission and vision." - ASHE [6]
For larger organizations, consider a multi-tiered approach. A central council can oversee broad strategies, while sub-committees focus on specific areas like energy, waste management, or clinical practices [4]. To ensure consistency, develop a shared sustainability glossary so all departments use the same language when discussing goals and metrics [4][6].
Once governance is in place, the next step is to define clear and measurable sustainability targets.
Creating SMART Sustainability Goals
Sustainability goals should follow the SMART framework: Specific, Measurable, Achievable, Relevant, and Time-bound. For instance, you might aim to cut red bag waste by 20% by December 31, 2026, which would also lead to notable cost savings [4].
Implement a Measurement and Verification (M&V) protocol early to track progress transparently and provide data-backed results to stakeholders like the CFO [4]. Begin with low-risk initiatives that deliver immediate results without affecting clinical care. For example, energy efficiency upgrades often yield quick savings. Conduct waste audits to identify items mistakenly placed in red bag waste that could be recycled or disposed of as general waste [4]. Additionally, collaborate with anesthesiologists to transition away from high-global warming potential gases, such as nitrous oxide, to alternatives like isoflurane [4].
These well-defined goals create a solid foundation for aligning sustainability efforts with both financial and clinical objectives.
Connecting Sustainability to Value-Based Care
Linking sustainability initiatives to value-based care can drive long-term health outcomes while reducing costs. Energy efficiency and waste reduction not only lower operational expenses but also contribute to healthier environments, enhancing patient care.
One effective strategy is to establish a "Climate Fund." Savings from low-cost interventions, such as automated HVAC adjustments or staff behavior changes, can be reinvested into high-impact sustainability projects [7]. Since fossil fuel emissions account for approximately 95% of a hospital's Scope 1 and 2 emissions, focusing on energy reduction offers a direct route to both decarbonization and cost savings [4]. This approach shows leadership and stakeholders that sustainability investments deliver measurable returns while advancing the organization’s mission of care and stewardship.
Selecting and Measuring Healthcare Sustainability Metrics
Healthcare Sustainability Benchmarking: Key Metrics and Performance Indicators
Once governance structures and goals are in place, the next step is to identify metrics that accurately measure progress. Having precise measurements transforms sustainability aspirations into tangible actions. As Elizabeth Schenk, PhD, RN, Chief Environmental Stewardship Officer at Providence, emphasizes:
"Educated guesses just don't have the same power as real numbers when it comes to driving change" [8].
These metrics serve as the foundation for evaluating sustainability efforts in a structured and meaningful way.
Key Performance Indicators (KPIs) for Healthcare
Healthcare organizations should focus on metrics across four key areas: environmental, clinical, social, and financial. For environmental performance, metrics like the Energy Use Index (EUI) - measured in kBtu per square foot annually - are critical. The national median for U.S. hospitals is 234.3 kBtu/sq. ft./year [8]. Other environmental indicators include water intensity (gallons per square foot) and waste diversion rates, which track the percentage of waste diverted from landfills.
Clinical metrics often target high-impact areas such as anesthetic gases. For instance, eliminating the use of desflurane can lower greenhouse gas emissions by 66% [5]. Social metrics focus on equity initiatives, with 85% of healthcare applicants in 2024 reporting the formation of internal racial equity committees, compared to 77% in 2023 [5]. Financial KPIs capture savings from sustainability projects, such as reduced landfill fees and returns on investments in efficiency improvements.
Metric Category | Key Performance Indicator (KPI) | Common Units |
|---|---|---|
Energy | Energy Use Index (EUI) | kBtu/sq. ft./year |
Water | Water Intensity | Gallons/sq. ft. |
Waste | Waste Optimization Score | % Diverted from Landfill |
Clinical | Anesthetic Gas Reduction | Metric tons CO₂e |
Social | Racial Equity Governance | % of facilities with committees |
Financial | Sustainability Savings | USD ($) |
Data Sources and Normalization Methods
After selecting metrics, the next challenge is gathering accurate data and ensuring fair comparisons. Data can be sourced from utility bills, waste invoices, electronic health records (EHRs), and supplier reports. However, raw numbers alone are insufficient. To provide meaningful insights, data should be standardized - whether by square footage, patient days, or full-time equivalent staff [8].
For example, Providence Seaside Hospital reduced its water consumption from 35.5 gallons per square foot in 2022 to 28.3 gallons per square foot by mid-2024, thanks to targeted facility upgrades led by Andy Mason, the hospital's facilities director [8]. This normalized metric allowed the leadership to compare performance across its 51-hospital network, leading to a $923,000 investment in water efficiency projects with an anticipated two-year payback period [8].
When integrating new data sources, allow two quarters for validation [8]. Additionally, push vendors to provide auditable electronic data rather than estimates. Geoffrey Glass, Senior Manager for Energy and Sustainability at Providence, explains:
"Within a minute you can tell what you're doing well and where you have opportunities to improve. We now benchmark using validated data" [8].
Equity and Risk-Adjusted Metrics
Not all healthcare facilities operate under the same conditions. Differences in patient populations, climate, and infrastructure mean that equity-sensitive and risk-adjusted metrics are essential. For example, hospitals with EUI scores below 150 often deliver lower-intensity care, while those exceeding 300 may operate in extreme climates or rely on outdated infrastructure [8].
Metrics should also account for patient complexity and social determinants of health. A hospital serving a high-acuity population will naturally consume more resources than an outpatient clinic. Between 2017 and 2020, Dr. Brian Chesebro at Providence discovered that while clinical use of nitrous oxide dropped by 61%, emissions from purchases remained high due to undetected leaks in central supply lines [8]. By comparing purchase data with EHR usage, the team identified discrepancies, switched to portable tanks at 17 hospitals, and reduced nitrous oxide purchases by 99%, cutting 4,000 metric tons of CO₂e annually [8]. This approach highlights how risk-adjusted analysis can uncover inefficiencies that traditional metrics might overlook, enabling organizations to set more realistic and impactful goals.
Benchmarking Against Internal and External Standards
Accurate metrics allow organizations to measure their performance and compare it against both internal benchmarks and industry standards, uncovering their current position and areas for growth.
Internal vs External Benchmarking
Internal benchmarking focuses on tracking progress within an organization over time or comparing performance across different facilities in a system [9][11]. This method is particularly useful for real-time evaluations of past and present performance, helping refine goals and direct resources effectively [3]. For instance, in a multi-site system, you might identify which locations excel in water conservation or waste reduction and replicate those successful practices across other sites.
External benchmarking, on the other hand, involves comparing your organization’s performance against peer institutions and national standards to identify gaps and opportunities [3][11]. This approach helps you stay informed about industry trends, assess the return on investment of strategies used by others, and adopt proven best practices [11]. By turning raw data into actionable insights, external benchmarking provides a broader perspective on where your organization stands.
Most organizations use a combination of both methods. Internal benchmarking ensures site-specific improvements and better resource management, while external benchmarking offers valuable context for how your performance measures up within the industry [3][11]. Together, these insights help guide the selection of effective benchmarking tools to achieve sustainability goals.
Using External Benchmarking Tools
Once key metrics are established, external benchmarking tools can validate and challenge your internal targets. One widely used tool in U.S. healthcare is the Practice Greenhealth Sustainability Benchmark Report, which allows hospitals to compare their performance with over 1,500 peer facilities [3][11]. Member hospitals receive annual report cards that benchmark their performance across 30 metrics [12]. These metrics span 11 impact areas, including leadership, waste, chemicals, operating room practices, food, energy, water, and climate [10][1].
Such benchmarks not only highlight potential savings and resource efficiencies but also provide early insights into Scope 3 emissions - those related to supply chain impacts. This data offers one of the first comprehensive glimpses into this critical area within the healthcare sector [5].
Organizations rely on these tools to conduct gap analyses, pinpointing areas where they fall behind industry medians or top-performing institutions [12]. Notably, 89% of respondents in 2023 reported having a sustainability leader at the health system level, and 62% of hospitals now report sustainability progress directly to their board of directors [13].
Applying Benchmarks to Set Targets
External benchmarks can also serve as a foundation for setting actionable and measurable targets. For example, using 90th percentile benchmarks enables organizations to establish ambitious long-term goals [12]. This data is also instrumental in securing investments from leadership. For instance, showing that eliminating desflurane led to a 66% reduction in greenhouse gas emissions provides a compelling argument for similar initiatives [5].
To maximize the impact of benchmarking, align these insights with broader organizational goals. This could mean linking sustainability objectives to value-based care models, community health needs assessments, or racial equity initiatives. For example, 26% of hospitals now include climate change considerations in their Community Health Needs Assessment process, while 85% have established internal racial equity committees - an increase from 77% in 2023 [5][13]. These connections ensure that sustainability efforts contribute meaningfully to the organization’s overall mission.
Turning Insights Into Action
Benchmarking data becomes truly valuable when it drives clear and prioritized actions that seamlessly integrate into existing systems. Below, we explore how to transform these insights into meaningful, actionable targets.
Setting Realistic and Ambitious Targets
Sustainability targets should strike a balance between ambition and practicality. Benchmarking data can guide the establishment of short-term achievements while laying the foundation for long-term transformational goals. For instance, if a facility's energy efficiency currently falls in the mid-range, a short-term goal might involve significant performance improvements within a year, paired with a longer-term aim to achieve near-top efficiency.
Focus on key resource areas - energy, water, waste, and materials - where the data reveals the most significant opportunities [3]. Break these targets into specific categories. For example, phasing out desflurane, a high-impact anesthetic gas, can dramatically reduce greenhouse gas emissions. Between 2020 and 2024, the percentage of hospitals eliminating desflurane nearly doubled, rising from 29.6% to 61.3%, underscoring how bold goals can inspire industry-wide progress [5]. In waste management, set diversion rate targets. In 2023, participating facilities successfully diverted over 328 million pounds of waste from landfills through recycling programs [5].
Prioritizing Initiatives by Impact
Once realistic targets are defined, prioritize initiatives that deliver the highest returns. Consider factors like financial impact, feasibility, and alignment with clinical priorities [6].
Organize efforts into four major areas: Transportation, Buildings & Energy Use, Anesthetic Gases, and Waste [2]. Within each category, address the largest contributors first. For example, fossil fuel emissions typically account for 95% of a hospital's Scope 1 and 2 emissions, making energy efficiency upgrades a logical starting point [4].
Engage multidisciplinary teams to identify quick, high-impact wins, such as fixing nitrous oxide leaks or upgrading lighting systems [4][6]. Conduct waste audits to uncover cost-saving opportunities. For example, reducing red bag waste can slash disposal costs significantly, as regulated medical waste is far more expensive to handle than general waste [4]. Similarly, addressing nitrous oxide tank leaks and switching to lower-impact anesthetic agents like isoflurane can effectively cut greenhouse gas emissions while controlling costs [4].
Adding Sustainability to Performance Management
Embedding sustainability metrics into daily performance management ensures continuous progress toward established goals. To drive accountability, sustainability goals should be integrated into existing performance systems. Appoint a sustainability champion with a clear reporting line to facility managers or department heads, supported by an executive sponsor from the C-suite [4]. This dual governance structure ensures both operational effectiveness and strategic alignment.
Create multidisciplinary green teams with clearly assigned tasks and regular, structured meetings [4]. In 2024, 85% of healthcare organizations reported forming internal committees focused on racial equity, up from 77% in 2023, demonstrating how formal structures can enhance accountability [5].
Implement a measurement and verification (M&V) protocol early to track savings and monitor progress [4]. This protocol should be adaptable to accommodate renovations or expansions. Digital tools, like the Energy to Care Dashboard, provide real-time energy performance tracking and help communicate progress toward sustainability goals [4][6].
Incorporate sustainability KPIs into executive scorecards and operational dashboards. Steven Rice, CHRO of The Bill & Melinda Gates Foundation, emphasizes the importance of actionable data:
"I believe that the data will set you free. At the end of the day, it's about how you turn those pieces of information into insights that will improve business" [3].
Align sustainability metrics with capital planning cycles, setting both short-term and long-term goals for energy, water, and waste reduction [4]. Use internal communication channels, such as newsletters, to share measurable energy savings and highlight staff contributions [4]. Publicizing achievements fosters momentum and reinforces the message that sustainability is a central organizational priority. When sustainability metrics are tracked alongside clinical quality and financial performance indicators, it reinforces that environmental stewardship is an integral part of the organization's mission [6].
Maintaining Continuous Improvement and Resilience
Sustainability benchmarking isn’t a one-and-done task; it’s an ongoing process that adjusts to new challenges, regulations, and opportunities. By embedding resilience into your sustainability efforts, you can better navigate both gradual changes and sudden disruptions.
Annual Benchmarking Cycles
Conducting an annual review helps maintain a clear, adaptable foundation for your sustainability goals. Structured reporting cycles, such as the Practice Greenhealth Environmental Excellence Awards, provide a framework to document progress and account for changes like facility renovations or equipment updates. Early implementation of a Measurement and Verification (M&V) protocol, alongside tools like the ASHE Energy to Care Dashboard, allows for real-time tracking and strategic adjustments [3][4][5].
The results speak volumes: in 2023, nearly 430 healthcare facilities participating in these cycles collectively saved over $182 million, reduced energy use by more than 1 billion kBtus, and diverted 328 million pounds of waste from landfills [5]. These reviews also help assess the effectiveness of targeted interventions. For instance, hospitals phasing out desflurane nearly doubled their progress from 29.6% in 2020 to 61.3% in 2024, cutting associated greenhouse gas emissions by 66% [5].
Beyond these scheduled reviews, preparing for unexpected events through scenario planning is essential to maintaining operational resilience.
Scenario Planning for Climate Resilience
With climate disruptions on the rise, scenario planning has become critical for safeguarding healthcare operations. This requires a multidisciplinary approach, bringing together teams from Facilities, Nursing, Supply Chain, Engineering, Sustainability, and Emergency Planning. These groups can integrate climate resilience into existing emergency preparedness and hazard vulnerability analyses (HVA) [15].
Reassess infrastructure capabilities to account for extreme weather events that exceed historical norms. For example, resilience plans should consider "black-start" and "islanding" capabilities, ensuring that critical services remain powered even during prolonged grid outages. On-site solar power paired with battery storage can provide a reliable energy source when both the grid and backup generators fail [17].
Tools like the HHS Administration for Strategic Preparedness and Response (ASPR) Risk Identification and Site Criticality (RISC) Toolkit can support forward-looking risk assessments [16]. Resilience planning should focus on key areas such as climate risk data, infrastructure protection, land use, clinical care continuity, and environmental safeguards [15]. Collaborating with community partners and government agencies ensures compliance with state-specific mandates, such as Washington State's Clean Buildings Law or New York's Climate Leadership and Community Protection Act [15][17].
As your resilience strategies evolve, so too should the metrics you use to measure progress.
Updating Metrics and Methods
Sustainability priorities shift over time, and your metrics need to keep pace. For instance, in 2024, 85% of healthcare organizations reported forming internal committees focused on racial equity - up from 77% in 2023 - showing how sustainability now encompasses social impact alongside environmental goals [5].
Expand your metrics to include Scope 3 emissions estimates and clinical waste data. In 2023, 49 facilities successfully eliminated harmful chemicals like PVC and DEHP from at least two medical product categories within two years [5]. Metrics should also account for potent greenhouse gases, such as refrigerants and nitrous oxide, which have significant global warming potential [4].
Real-time data analysis is essential for making informed decisions quickly [3]. Adding qualitative insights to your benchmarking data - such as explanations of performance trends, areas of high resource use, or planned efficiency projects - can provide valuable context. This narrative approach helps stakeholders see the bigger picture and builds support for future initiatives [14].
At Council Fire (https://councilfire.org), we emphasize an integrated strategy - combining regular benchmarking, proactive scenario planning, and evolving metrics to create lasting sustainability in healthcare.
Conclusion
Achieving sustainability in healthcare demands a well-structured approach, combining clear governance, aligned objectives, and a commitment to continuous improvement. The numbers speak for themselves: organizations that adopt comprehensive sustainability practices can cut operational costs by as much as 30% through enhanced efficiency and waste reduction [3].
The role of an engaged workforce cannot be overstated. Success hinges on staff who not only understand the goals but also receive proper training and see tangible results. Formal green teams - comprising members from both executive leadership and frontline staff - can unify efforts toward shared sustainability objectives.
The importance of setting SMART goals and conducting regular benchmarking is highlighted by the Joint Commission, which emphasizes accountability and strategic alignment [2]. These practices form the backbone of a cyclical process, encompassing goal-setting and continuous refinement.
Sustainability is a dynamic endeavor. Metrics and methodologies must adapt to emerging challenges, leveraging tools like real-time data analytics to make swift, informed decisions. This flexibility ensures strategies remain relevant and capitalize on new opportunities as they arise.
"I believe that the data will set you free. At the end of the day, it's about how you turn those pieces of information into insights that will improve business" [3].
Steven Rice, CHRO at The Bill & Melinda Gates Foundation
FAQs
How can healthcare organizations track and measure their sustainability goals effectively?
To effectively measure progress in sustainability, healthcare organizations should begin by gathering baseline data. This involves assessing direct emissions (Scope 1), indirect emissions from energy usage (Scope 2), and broader supply chain impacts (Scope 3), as categorized by the Greenhouse Gas Protocol. Conducting facility assessments, energy and waste audits, and supply chain inventories can provide the necessary information. Converting measurements such as kilowatt-hours, gallons, or cubic feet into CO₂e equivalents allows for meaningful year-over-year comparisons.
Once the baseline is established, organizations can measure their performance against industry benchmarks, like those found in Practice Greenhealth’s annual Sustainability Benchmark Report. Regular updates to dashboards with real-time or monthly data - covering metrics like energy savings, water use reduction, or waste management - enable organizations to turn raw numbers into actionable insights. Tools such as the ENERGY STAR® Portfolio Manager can simplify the process of tracking and reporting.
Council Fire offers strategic support to healthcare organizations in areas like data collection, fostering collaboration among stakeholders, and communicating progress. By leveraging standardized methods and benchmarking tools, hospitals can achieve tangible results, such as cutting CO₂e emissions by 15% or saving $1.2 million annually, all while contributing to national climate objectives.
What challenges do healthcare organizations face when setting SMART sustainability goals?
Healthcare organizations face a range of obstacles when attempting to establish SMART (Specific, Measurable, Achievable, Relevant, Time-bound) sustainability goals. A primary issue is the absence of reliable baseline data. Many facilities find it challenging to accurately track direct emissions (Scope 1) and indirect emissions from purchased energy (Scope 2). Tackling Scope 3 emissions - such as those from supply chain operations, waste management, and employee commuting - proves even more difficult. Without dependable data, creating measurable and verifiable goals becomes a daunting task.
Another significant hurdle is the lack of consistent industry benchmarks. While some organizations report notable savings, individual facilities often lack a standardized way to evaluate their performance against similar institutions. This gap makes it harder to set targets that are both realistic and ambitious. Adding to the complexity, fragmented reporting standards across the industry further hinder progress.
Lastly, gaining alignment among diverse stakeholders poses a challenge. Clinicians, facility managers, procurement teams, and leadership often have differing priorities, and internal silos can obstruct collaboration. Successful sustainability strategies demand teamwork, transparency, and unified goals, yet competing agendas frequently slow momentum. Overcoming these barriers is essential for achieving impactful sustainability results.
How can healthcare facilities align sustainability goals with value-based care models?
Healthcare facilities can weave sustainability goals into value-based care (VBC) models by incorporating environmental performance into their assessments of quality and cost. By monitoring data such as energy usage, waste production, water consumption, and supply chain emissions alongside clinical outcomes and expenses, hospitals can measure the financial and environmental benefits of eco-friendly initiatives. For instance, efforts like reducing utility bills or cutting waste disposal costs can directly contribute to both cost savings and improved care quality.
Collaboration plays a crucial role in making this integration effective. Engaging clinicians, payers, and patients in setting benchmarks allows facilities to align sustainability goals with reimbursement incentives. For example, cutting back on carbon-heavy practices - such as minimizing energy-intensive equipment use or addressing emissions from supply chains - can lead to better care at lower costs. Transparent reporting of these outcomes helps build trust and enables payers to reward facilities that achieve both clinical and environmental objectives.
Working with sustainability-focused organizations like Council Fire provides healthcare systems with the tools and strategies needed to balance financial goals with environmental and social progress. These partnerships bring the expertise required to embed sustainable practices into performance metrics, fostering ongoing improvements in both healthcare delivery and environmental stewardship.
Related Blog Posts

FAQ
What does it really mean to “redefine profit”?
What makes Council Fire different?
Who does Council Fire you work with?
What does working with Council Fire actually look like?
How does Council Fire help organizations turn big goals into action?
How does Council Fire define and measure success?


