

Sep 25, 2025
Sep 25, 2025
Ultimate Guide to Energy Efficiency in Healthcare
Sustainability Strategy
Sustainability Strategy
In This Article
Explore effective energy efficiency strategies for healthcare facilities that enhance patient care while reducing costs and environmental impact.
Ultimate Guide to Energy Efficiency in Healthcare
Healthcare facilities consume about 9% of the energy used by commercial buildings in the U.S., despite occupying only 4% of the total commercial floorspace. This makes energy efficiency a critical focus for cost reduction, patient care, and environmental responsibility. By upgrading systems like HVAC, lighting, and building insulation, hospitals can reduce energy use by up to 30% without compromising safety or comfort.
Key Takeaways:
Energy Audits: Identify inefficiencies and benchmark against industry standards.
Building Upgrades: Improve insulation, seal air leaks, and install energy-efficient windows.
System Optimization: Transition to LED lighting, use smart HVAC controls, and implement energy recovery systems.
Renewable Energy: Integrate solar panels, combined heat and power systems, or geothermal solutions.
Stakeholder Collaboration: Engage facility managers, medical staff, and administrators to align energy goals with operational needs.
Implementation Strategies: Minimize disruptions with phased upgrades, temporary redundancies, and rigorous system testing.
Long-term success depends on regular monitoring, preventive maintenance, and post-upgrade evaluations to ensure systems perform as planned. With proper planning and execution, healthcare facilities can achieve energy efficiency while maintaining high standards of patient care and operational reliability.
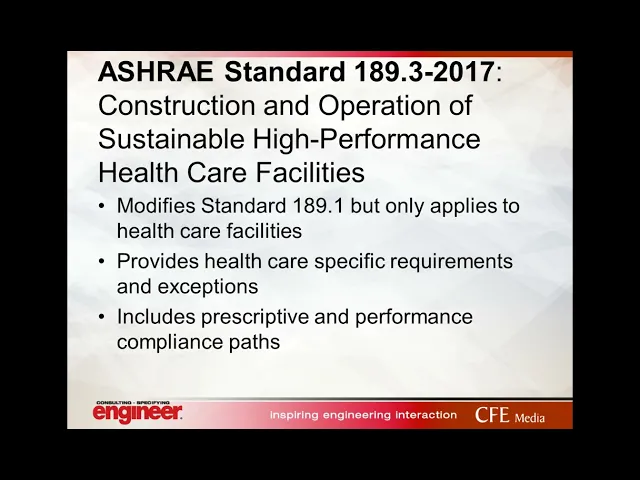
HVAC: Hospitals and health care facilities
Energy Assessment and Planning
Laying the groundwork for energy efficiency in healthcare facilities starts with thorough assessment and well-thought-out planning. These steps ensure that investments not only yield strong returns but also support the uninterrupted operations critical to patient care. The planning phase demands collaboration across various stakeholders and often benefits from expert guidance to address the unique needs of healthcare environments. Below, we explore the key components of energy audits and the role of stakeholder engagement in driving meaningful improvements.
Energy Audits and Benchmarking
In healthcare, where operations run around the clock and regulatory demands are high, energy audits are an essential tool. These audits assess facility systems by comparing their performance to design specifications or the most effective technologies available [2]. For hospitals and clinics, this evaluation is vital to achieving energy efficiency without compromising patient care.
Auditors rely on utility data, building blueprints, and system evaluations to establish a performance baseline. This baseline allows facilities to track progress, spot trends, and refine energy practices over time [2][3][5]. The potential for improvement is striking: hospitals could save up to 30% of their energy use without sacrificing comfort or safety by adopting best practices and upgrading to efficient systems [4]. This is particularly significant given that healthcare facilities in the U.S. account for about 9% of energy consumption in commercial buildings, despite occupying just 4% of the total commercial floorspace [4].
Benchmarking adds another layer of insight by comparing a facility's energy use intensity with regional and national averages. This contextual analysis highlights specific areas where improvements can be made, helping facilities prioritize their energy goals.
Stakeholder Engagement and Goal Setting
Effective energy planning hinges on the involvement of a wide range of stakeholders. From straightforward behavioral adjustments to complex system overhauls, achieving alignment among these groups is critical for success [1].
Facility managers bring operational insight and knowledge of existing systems, enabling them to identify and prioritize improvement opportunities.
Medical staff ensure that patient care remains the top priority, particularly in areas like operating rooms and intensive care units where stable conditions are non-negotiable.
Administrative leaders provide the financial backing and strategic vision to integrate energy goals with broader institutional objectives.
Setting goals for energy efficiency involves balancing ambition with practicality. Both short- and long-term objectives should be clearly defined, with mechanisms for measuring and verifying progress built into the plan. This collaborative approach ensures that all parties are aligned and ready to work toward shared outcomes.
Working with Consultants for Planning
Expert consultants can play a pivotal role in crafting effective energy strategies for healthcare facilities. Their specialized knowledge ensures that plans align with U.S. standards and industry best practices. Through detailed audits, consultants help identify opportunities for high-return investments and energy conservation [2]. They also bring a fresh perspective, often uncovering opportunities that internal teams might miss, and help avoid common pitfalls during implementation.
Organizations like Council Fire offer end-to-end support, combining financial considerations with environmental and operational goals. Their expertise helps healthcare facilities design energy strategies that improve efficiency while supporting sustainability objectives.
When choosing a consultant, healthcare organizations should prioritize firms with proven technical expertise and a track record in the healthcare sector. Deliverables such as detailed energy models, prioritized action plans, and ongoing performance monitoring should be part of the package, ensuring a clear and actionable path forward.
Key Energy Efficiency Measures
Once assessments are complete and goals are defined, the next step is implementing targeted measures in three main areas: improving the building envelope, optimizing lighting and HVAC systems, and incorporating renewable energy solutions. These steps transform planning into tangible energy savings while addressing the unique operational needs of healthcare facilities.
Building Envelope Improvements
The building envelope serves as the primary barrier against energy loss, making it a critical focus for efficiency upgrades in healthcare settings. Enhancing insulation, installing energy-efficient windows with low-emissivity coatings, and sealing gaps are practical ways to reduce HVAC demands and improve indoor comfort.
Upgrading insulation is among the most cost-effective strategies, especially when tailored to the climate zone of the facility. Better-insulated walls and roofs reduce the workload on mechanical systems, allowing them to operate more efficiently.
Air sealing is equally important. By closing gaps around penetrations, joints, and other connections, facilities can minimize energy loss and maintain precise pressure relationships - an essential factor in healthcare environments where air quality and infection control are priorities. Using the right materials for sealing ensures both energy efficiency and compliance with indoor air quality standards.
These envelope improvements work hand-in-hand with HVAC systems, enabling them to perform more effectively with reduced strain and lower maintenance requirements.
Lighting and HVAC System Optimization
Lighting and HVAC systems are major energy consumers in healthcare facilities, making their optimization a key area for improvement. The transition to LED lighting offers significant benefits, including lower energy consumption, longer lifespan, and excellent light quality. Adding controls such as occupancy sensors and daylight-responsive systems further reduces energy use in areas with variable occupancy.
For HVAC systems, upgrades can deliver substantial energy savings while maintaining the high performance required in healthcare settings. Installing variable frequency drives on motors and fans allows systems to adjust output based on real-time needs, improving efficiency. Smart building automation systems provide continuous monitoring and adjustments, ensuring optimal performance and reducing waste.
Energy recovery ventilation systems are another valuable addition. These systems capture heat and moisture from exhaust air to pre-condition incoming fresh air, which is particularly beneficial in healthcare facilities where high ventilation rates are essential for infection control.
Renewable Energy Solutions
Renewable energy solutions complement efficiency upgrades by reducing reliance on grid power and lowering operational costs. Solar photovoltaic systems, for example, can be installed on rooftops or over parking areas, aligning well with daytime energy demands. These systems often have a short payback period, thanks to reduced electricity expenses.
Other renewable options include combined heat and power (CHP) systems, which generate electricity while utilizing waste heat for space heating or hot water needs. Thermal energy storage systems, such as ice storage, allow facilities to store cooling capacity during off-peak hours and use it during peak demand. Geothermal heat pump systems leverage stable underground temperatures to provide energy-efficient heating and cooling.
To ensure these renewable systems integrate seamlessly with existing infrastructure, careful planning is essential. Coordination with backup power systems is particularly important to guarantee uninterrupted operation of critical healthcare systems.
Implementation and Quality Assurance
After thorough planning and evaluation, the next critical step in energy upgrades is executing them with minimal disruption while ensuring systems perform as intended. In healthcare settings, this phase demands precise coordination to maintain patient safety and operational continuity. Success hinges on careful planning, rigorous testing, and continuous monitoring to confirm that upgrades meet design and performance expectations.
Reducing Disruptions During Implementation
To avoid interrupting patient care, energy projects are often carried out in phases. This approach allows work to proceed in specific sections while other areas of the facility remain fully operational.
Temporary redundancies are essential for critical systems undergoing upgrades. For example, portable HVAC units can maintain climate control in patient areas while permanent systems are being updated. Scheduling non-critical upgrades during nights and weekends further minimizes disruptions, and daily staff briefings help everyone navigate temporary changes efficiently.
Clear signage and designated alternative routes ensure that staff and patients can move safely around construction zones without affecting care delivery. Emergency preparedness also becomes a top priority during this phase: backup power systems should remain fully functional, and life safety systems must be continuously monitored. Installing temporary monitoring systems provides real-time alerts if critical systems experience interruptions.
Collaboration with infection control teams is vital to maintain sterile environments during construction. Measures like negative pressure barriers, dust containment systems, and specialized ventilation are crucial for maintaining air quality in sensitive areas such as operating rooms and intensive care units.
Commissioning and Performance Verification
Commissioning is the process of validating that all systems meet their design specifications and operational requirements. This involves testing individual components before integrating them into the larger system.
Initial testing focuses on functional checks for components like motors, fans, pumps, and control devices to ensure they meet performance standards. Calibration of temperature sensors, pressure gauges, and airflow meters ensures accurate readings, which are critical for ongoing operations.
Building automation systems play a key role by continuously monitoring energy use, efficiency, and environmental conditions. Real-time data collection enables facility managers to quickly identify and address performance issues.
Staff training is another essential part of commissioning. Maintenance teams are trained on operating procedures, troubleshooting methods, and routine maintenance schedules. Detailed documentation, including operating manuals, warranty information, and maintenance plans, ensures that teams have the resources they need to manage the upgraded systems effectively.
Performance verification extends beyond initial testing. By analyzing trends over the first several months, facility managers can identify seasonal variations, usage patterns, and opportunities for system adjustments that may not have been evident during commissioning.
Post-Occupancy Evaluation for Improvement
Post-occupancy evaluations provide critical feedback on how energy efficiency measures perform under real-world conditions. Conducted 12 to 18 months after project completion, these assessments allow time for systems to stabilize and for staff to adapt to new procedures.
Energy consumption data is compared with initial projections to confirm whether efficiency goals are being met. Utility bills and automation system data offer a clear picture of actual performance. If significant deviations arise, they are investigated to determine the cause.
Indoor environmental quality is also assessed to ensure that energy upgrades haven't negatively impacted patient comfort or clinical operations. Metrics like temperature, humidity, and air quality are monitored to confirm that the facility meets required standards.
Staff feedback collected through surveys and interviews offers insights that technical data might overlook. This input often reveals small adjustments that can enhance both energy performance and user satisfaction.
The evaluation process also examines maintenance needs and operational costs. Comparing actual maintenance requirements to initial projections helps refine future planning. A cost-benefit analysis updates financial models with real-world data, providing a more accurate foundation for future energy projects.
Organizations like Council Fire bring specialized expertise to post-occupancy evaluations, helping healthcare facilities analyze performance data and identify further opportunities for system optimization. Their experience with energy and water infrastructure projects ensures a thorough assessment and actionable recommendations.
Quarterly performance reviews track key indicators, highlighting any trends that could signal equipment wear or operational changes. This ongoing evaluation helps maintain energy efficiency benefits while ensuring the facility continues to meet the high standards of patient care. By continuously refining processes, healthcare facilities can sustain long-term efficiency and improve outcomes for future projects.
Operations, Maintenance, and Monitoring
Maintaining energy efficiency in healthcare facilities requires integrating operations, maintenance, and consistent monitoring into everyday management. Facilities that excel in sustaining energy performance make energy awareness a fundamental part of their daily decision-making and operational processes.
Maintaining Energy Performance
Ongoing staff training, combined with real-time Energy Management Systems (EMS), equips maintenance teams with the tools and knowledge to keep efficiency on track. These systems use data analytics to detect trends, such as equipment wear or seasonal shifts in efficiency, that might otherwise go unnoticed with manual checks.
"Energy Management Systems (EMS) play a pivotal role in the real-time monitoring and control of energy usage within healthcare facilities. These systems provide granular insights into consumption patterns, identify areas of high energy use, and facilitate proactive energy management."
American Hospital & Healthcare Management [3]
Preventive maintenance schedules are key to ensuring that equipment like HVAC systems, lighting controls, and building automation components operate efficiently. Regular cleaning and calibration prevent energy waste caused by neglect or deferred maintenance.
Modern monitoring devices can track electricity, water usage, and room temperatures with impressive precision. While some devices may require a higher upfront investment, their accuracy and reliability often justify the cost. For example, plug-in monitors are ideal for individual equipment, while clamp-on systems provide insights into entire building circuits or specific electrical panels. Depending on the complexity of the setup, professional installation may be necessary, so planning and budgeting for such expertise is essential.
By adopting these monitoring practices, facilities can embed a culture of energy-conscious management into their operations.
Embedding Sustainability in Facility Management
Sustainability thrives when it becomes an integral part of management practices. Incorporating energy efficiency into performance systems encourages ongoing improvement and accountability. For example, energy efficiency metrics can be included in staff evaluations and departmental budgets, ensuring everyone plays a role in achieving sustainability goals.
Building on this, improvement cycles - like monthly energy reviews - help teams spot inefficiencies early by analyzing utility bills, automation system data, and maintenance logs. These reviews provide opportunities to address anomalies before they escalate into larger issues.
Designating energy champions within departments can further reinforce energy-conscious behaviors. Acting as liaisons between their teams and facility management, these individuals cultivate a widespread commitment to energy efficiency across the organization.
Procurement decisions also play a role in sustaining efficiency. When replacing equipment or supplies, prioritizing energy-efficient options alongside cost and functionality ensures long-term gains. These efforts, paired with robust documentation and reporting systems, help track progress against established benchmarks. Regular reporting not only informs budget planning but also supports future investments in efficiency improvements.
Regular Reviews and Adjustments
Routine reviews are essential for tracking energy performance indicators and identifying deviations in usage, equipment functionality, and maintenance expenses. Seasonal adjustments, such as modifying HVAC settings or lighting schedules, ensure facilities adapt to changing weather and occupancy levels without sacrificing efficiency or patient care.
Organizations like Council Fire offer specialized expertise in energy performance reviews, helping healthcare facilities analyze complex data and uncover opportunities for optimization. Their balanced approach integrates financial planning with sustainability efforts, ensuring both cost control and environmental goals are met.
Staying up to date with technology advancements is equally important. New building automation software, monitoring devices, and control systems can enhance functionality and improve efficiency. Regularly evaluating these updates keeps facilities at the forefront of energy management.
Benchmarking performance against industry standards provides valuable context, revealing whether current practices align with best practices or need adjustment. Comparing metrics like energy use intensity against similar facilities can highlight areas for improvement.
Finally, user-friendly monitoring systems with accessible mobile or web interfaces encourage staff engagement. When data is easy to process and analyze, teams can quickly identify and address issues, ensuring continuous improvements in energy efficiency.
Conclusion and Key Takeaways
Energy efficiency in healthcare facilities goes beyond simply cutting costs - it plays a pivotal role in improving financial performance, enhancing clinical outcomes, and addressing environmental concerns. Achieving meaningful results requires teamwork across the organization, from leadership to frontline staff.
Highlights of Energy Efficiency Benefits
Reducing energy consumption leads to lower utility expenses, increased reliability of equipment, and decreased maintenance costs, which can free up resources for other facility improvements. Modern HVAC systems and advanced building automation technologies optimize energy use while ensuring precise climate control - an essential factor for patient recovery and staff productivity. Additionally, upgraded lighting systems improve visibility in critical areas while consuming less energy.
The environmental benefits are equally compelling. Lower energy usage translates to a reduced carbon footprint and contributes to cleaner air in the surrounding community, aligning with the values of patients, staff, and local stakeholders. Enhanced indoor conditions, such as better temperature consistency, improved air quality, and quieter operations, also create a more conducive healing environment, reinforcing the facility's commitment to comprehensive care.
Moving Forward with Implementation
Once the groundwork has been laid through assessments and initial steps, the focus shifts to ensuring these energy efficiencies deliver lasting value. Long-term planning is crucial to meet evolving demands and incorporate emerging technologies.
Engaging stakeholders is a cornerstone of successful implementation. Gaining buy-in from clinical teams, facility managers, financial planners, and executive leaders ensures that energy initiatives are well-supported and properly resourced. Regular updates and communication help maintain enthusiasm and encourage ongoing participation.
Expert guidance can simplify the process. Organizations like Council Fire provide valuable expertise in integrating energy efficiency with financial and operational goals. Their collaborative strategies help healthcare facilities navigate the complexities of energy management, ensuring alignment with broader objectives while maximizing both cost savings and environmental benefits.
As energy management tools and technologies continue to advance, healthcare facilities with robust practices - such as thorough monitoring, consistent maintenance, staff training, and performance evaluations - will be well-positioned to seize new opportunities and maintain leadership in energy efficiency.
Achieving optimal energy efficiency is a continuous journey. By committing to a well-rounded and deliberate approach, healthcare facilities can secure long-term financial returns, enhance patient care, and contribute positively to their communities. These efforts not only support sustainable healthcare practices but also strengthen the facility’s position as a leader in energy-conscious operations.
FAQs
What are the most affordable ways for healthcare facilities to improve energy efficiency without affecting patient care?
Healthcare facilities can take practical steps to improve energy efficiency without interfering with patient care. For instance, switching to LED lighting can significantly cut energy use while providing reliable illumination. Installing motion sensors to automate lighting and HVAC systems further reduces unnecessary energy consumption. Addressing issues like leaks in steam and water systems is another straightforward way to prevent waste.
Another effective measure is the use of variable frequency drives on equipment, which helps adjust energy use to match operational needs without sacrificing performance. These strategies are budget-friendly and simple to implement, allowing facilities to lower energy costs while maintaining a safe and comfortable environment for both patients and staff.
How can healthcare facilities improve energy efficiency without compromising indoor air quality or infection control?
Healthcare facilities can improve energy efficiency without compromising indoor air quality or infection control by using high-efficiency air filtration systems like HEPA filters or UV germicidal irradiation (UVGI). These advanced systems effectively reduce airborne pathogens while maintaining energy-efficient airflow.
Facilities can also fine-tune ventilation by adjusting outdoor air intake and limiting unnecessary air exchanges during times of low occupancy. This approach saves energy while ensuring adequate airflow, as long as the systems are thoughtfully designed, regularly monitored, and properly maintained. Routine evaluations and updates to HVAC systems are crucial to achieving the right balance between energy efficiency and safety standards.
Why are energy audits important for improving energy efficiency in healthcare facilities?
Energy audits are essential for healthcare facilities aiming to improve energy efficiency. These assessments offer a detailed examination of energy consumption, highlighting inefficiencies and creating a foundation for monitoring progress.
By uncovering precise areas where savings are possible, facilities can establish practical, measurable goals and focus on the most impactful energy-saving strategies. This approach not only lowers operational expenses but also supports better resource management and sustainability - key priorities in the energy-demanding healthcare industry.
Related Blog Posts

Latest Articles
©2025
FAQ
FAQ
01
What does it really mean to “redefine profit”?
02
What makes Council Fire different?
03
Who does Council Fire you work with?
04
What does working with Council Fire actually look like?
05
How does Council Fire help organizations turn big goals into action?
06
How does Council Fire define and measure success?
01
What does it really mean to “redefine profit”?
02
What makes Council Fire different?
03
Who does Council Fire you work with?
04
What does working with Council Fire actually look like?
05
How does Council Fire help organizations turn big goals into action?
06
How does Council Fire define and measure success?


Sep 25, 2025
Ultimate Guide to Energy Efficiency in Healthcare
Sustainability Strategy
In This Article
Explore effective energy efficiency strategies for healthcare facilities that enhance patient care while reducing costs and environmental impact.
Ultimate Guide to Energy Efficiency in Healthcare
Healthcare facilities consume about 9% of the energy used by commercial buildings in the U.S., despite occupying only 4% of the total commercial floorspace. This makes energy efficiency a critical focus for cost reduction, patient care, and environmental responsibility. By upgrading systems like HVAC, lighting, and building insulation, hospitals can reduce energy use by up to 30% without compromising safety or comfort.
Key Takeaways:
Energy Audits: Identify inefficiencies and benchmark against industry standards.
Building Upgrades: Improve insulation, seal air leaks, and install energy-efficient windows.
System Optimization: Transition to LED lighting, use smart HVAC controls, and implement energy recovery systems.
Renewable Energy: Integrate solar panels, combined heat and power systems, or geothermal solutions.
Stakeholder Collaboration: Engage facility managers, medical staff, and administrators to align energy goals with operational needs.
Implementation Strategies: Minimize disruptions with phased upgrades, temporary redundancies, and rigorous system testing.
Long-term success depends on regular monitoring, preventive maintenance, and post-upgrade evaluations to ensure systems perform as planned. With proper planning and execution, healthcare facilities can achieve energy efficiency while maintaining high standards of patient care and operational reliability.
HVAC: Hospitals and health care facilities
Energy Assessment and Planning
Laying the groundwork for energy efficiency in healthcare facilities starts with thorough assessment and well-thought-out planning. These steps ensure that investments not only yield strong returns but also support the uninterrupted operations critical to patient care. The planning phase demands collaboration across various stakeholders and often benefits from expert guidance to address the unique needs of healthcare environments. Below, we explore the key components of energy audits and the role of stakeholder engagement in driving meaningful improvements.
Energy Audits and Benchmarking
In healthcare, where operations run around the clock and regulatory demands are high, energy audits are an essential tool. These audits assess facility systems by comparing their performance to design specifications or the most effective technologies available [2]. For hospitals and clinics, this evaluation is vital to achieving energy efficiency without compromising patient care.
Auditors rely on utility data, building blueprints, and system evaluations to establish a performance baseline. This baseline allows facilities to track progress, spot trends, and refine energy practices over time [2][3][5]. The potential for improvement is striking: hospitals could save up to 30% of their energy use without sacrificing comfort or safety by adopting best practices and upgrading to efficient systems [4]. This is particularly significant given that healthcare facilities in the U.S. account for about 9% of energy consumption in commercial buildings, despite occupying just 4% of the total commercial floorspace [4].
Benchmarking adds another layer of insight by comparing a facility's energy use intensity with regional and national averages. This contextual analysis highlights specific areas where improvements can be made, helping facilities prioritize their energy goals.
Stakeholder Engagement and Goal Setting
Effective energy planning hinges on the involvement of a wide range of stakeholders. From straightforward behavioral adjustments to complex system overhauls, achieving alignment among these groups is critical for success [1].
Facility managers bring operational insight and knowledge of existing systems, enabling them to identify and prioritize improvement opportunities.
Medical staff ensure that patient care remains the top priority, particularly in areas like operating rooms and intensive care units where stable conditions are non-negotiable.
Administrative leaders provide the financial backing and strategic vision to integrate energy goals with broader institutional objectives.
Setting goals for energy efficiency involves balancing ambition with practicality. Both short- and long-term objectives should be clearly defined, with mechanisms for measuring and verifying progress built into the plan. This collaborative approach ensures that all parties are aligned and ready to work toward shared outcomes.
Working with Consultants for Planning
Expert consultants can play a pivotal role in crafting effective energy strategies for healthcare facilities. Their specialized knowledge ensures that plans align with U.S. standards and industry best practices. Through detailed audits, consultants help identify opportunities for high-return investments and energy conservation [2]. They also bring a fresh perspective, often uncovering opportunities that internal teams might miss, and help avoid common pitfalls during implementation.
Organizations like Council Fire offer end-to-end support, combining financial considerations with environmental and operational goals. Their expertise helps healthcare facilities design energy strategies that improve efficiency while supporting sustainability objectives.
When choosing a consultant, healthcare organizations should prioritize firms with proven technical expertise and a track record in the healthcare sector. Deliverables such as detailed energy models, prioritized action plans, and ongoing performance monitoring should be part of the package, ensuring a clear and actionable path forward.
Key Energy Efficiency Measures
Once assessments are complete and goals are defined, the next step is implementing targeted measures in three main areas: improving the building envelope, optimizing lighting and HVAC systems, and incorporating renewable energy solutions. These steps transform planning into tangible energy savings while addressing the unique operational needs of healthcare facilities.
Building Envelope Improvements
The building envelope serves as the primary barrier against energy loss, making it a critical focus for efficiency upgrades in healthcare settings. Enhancing insulation, installing energy-efficient windows with low-emissivity coatings, and sealing gaps are practical ways to reduce HVAC demands and improve indoor comfort.
Upgrading insulation is among the most cost-effective strategies, especially when tailored to the climate zone of the facility. Better-insulated walls and roofs reduce the workload on mechanical systems, allowing them to operate more efficiently.
Air sealing is equally important. By closing gaps around penetrations, joints, and other connections, facilities can minimize energy loss and maintain precise pressure relationships - an essential factor in healthcare environments where air quality and infection control are priorities. Using the right materials for sealing ensures both energy efficiency and compliance with indoor air quality standards.
These envelope improvements work hand-in-hand with HVAC systems, enabling them to perform more effectively with reduced strain and lower maintenance requirements.
Lighting and HVAC System Optimization
Lighting and HVAC systems are major energy consumers in healthcare facilities, making their optimization a key area for improvement. The transition to LED lighting offers significant benefits, including lower energy consumption, longer lifespan, and excellent light quality. Adding controls such as occupancy sensors and daylight-responsive systems further reduces energy use in areas with variable occupancy.
For HVAC systems, upgrades can deliver substantial energy savings while maintaining the high performance required in healthcare settings. Installing variable frequency drives on motors and fans allows systems to adjust output based on real-time needs, improving efficiency. Smart building automation systems provide continuous monitoring and adjustments, ensuring optimal performance and reducing waste.
Energy recovery ventilation systems are another valuable addition. These systems capture heat and moisture from exhaust air to pre-condition incoming fresh air, which is particularly beneficial in healthcare facilities where high ventilation rates are essential for infection control.
Renewable Energy Solutions
Renewable energy solutions complement efficiency upgrades by reducing reliance on grid power and lowering operational costs. Solar photovoltaic systems, for example, can be installed on rooftops or over parking areas, aligning well with daytime energy demands. These systems often have a short payback period, thanks to reduced electricity expenses.
Other renewable options include combined heat and power (CHP) systems, which generate electricity while utilizing waste heat for space heating or hot water needs. Thermal energy storage systems, such as ice storage, allow facilities to store cooling capacity during off-peak hours and use it during peak demand. Geothermal heat pump systems leverage stable underground temperatures to provide energy-efficient heating and cooling.
To ensure these renewable systems integrate seamlessly with existing infrastructure, careful planning is essential. Coordination with backup power systems is particularly important to guarantee uninterrupted operation of critical healthcare systems.
Implementation and Quality Assurance
After thorough planning and evaluation, the next critical step in energy upgrades is executing them with minimal disruption while ensuring systems perform as intended. In healthcare settings, this phase demands precise coordination to maintain patient safety and operational continuity. Success hinges on careful planning, rigorous testing, and continuous monitoring to confirm that upgrades meet design and performance expectations.
Reducing Disruptions During Implementation
To avoid interrupting patient care, energy projects are often carried out in phases. This approach allows work to proceed in specific sections while other areas of the facility remain fully operational.
Temporary redundancies are essential for critical systems undergoing upgrades. For example, portable HVAC units can maintain climate control in patient areas while permanent systems are being updated. Scheduling non-critical upgrades during nights and weekends further minimizes disruptions, and daily staff briefings help everyone navigate temporary changes efficiently.
Clear signage and designated alternative routes ensure that staff and patients can move safely around construction zones without affecting care delivery. Emergency preparedness also becomes a top priority during this phase: backup power systems should remain fully functional, and life safety systems must be continuously monitored. Installing temporary monitoring systems provides real-time alerts if critical systems experience interruptions.
Collaboration with infection control teams is vital to maintain sterile environments during construction. Measures like negative pressure barriers, dust containment systems, and specialized ventilation are crucial for maintaining air quality in sensitive areas such as operating rooms and intensive care units.
Commissioning and Performance Verification
Commissioning is the process of validating that all systems meet their design specifications and operational requirements. This involves testing individual components before integrating them into the larger system.
Initial testing focuses on functional checks for components like motors, fans, pumps, and control devices to ensure they meet performance standards. Calibration of temperature sensors, pressure gauges, and airflow meters ensures accurate readings, which are critical for ongoing operations.
Building automation systems play a key role by continuously monitoring energy use, efficiency, and environmental conditions. Real-time data collection enables facility managers to quickly identify and address performance issues.
Staff training is another essential part of commissioning. Maintenance teams are trained on operating procedures, troubleshooting methods, and routine maintenance schedules. Detailed documentation, including operating manuals, warranty information, and maintenance plans, ensures that teams have the resources they need to manage the upgraded systems effectively.
Performance verification extends beyond initial testing. By analyzing trends over the first several months, facility managers can identify seasonal variations, usage patterns, and opportunities for system adjustments that may not have been evident during commissioning.
Post-Occupancy Evaluation for Improvement
Post-occupancy evaluations provide critical feedback on how energy efficiency measures perform under real-world conditions. Conducted 12 to 18 months after project completion, these assessments allow time for systems to stabilize and for staff to adapt to new procedures.
Energy consumption data is compared with initial projections to confirm whether efficiency goals are being met. Utility bills and automation system data offer a clear picture of actual performance. If significant deviations arise, they are investigated to determine the cause.
Indoor environmental quality is also assessed to ensure that energy upgrades haven't negatively impacted patient comfort or clinical operations. Metrics like temperature, humidity, and air quality are monitored to confirm that the facility meets required standards.
Staff feedback collected through surveys and interviews offers insights that technical data might overlook. This input often reveals small adjustments that can enhance both energy performance and user satisfaction.
The evaluation process also examines maintenance needs and operational costs. Comparing actual maintenance requirements to initial projections helps refine future planning. A cost-benefit analysis updates financial models with real-world data, providing a more accurate foundation for future energy projects.
Organizations like Council Fire bring specialized expertise to post-occupancy evaluations, helping healthcare facilities analyze performance data and identify further opportunities for system optimization. Their experience with energy and water infrastructure projects ensures a thorough assessment and actionable recommendations.
Quarterly performance reviews track key indicators, highlighting any trends that could signal equipment wear or operational changes. This ongoing evaluation helps maintain energy efficiency benefits while ensuring the facility continues to meet the high standards of patient care. By continuously refining processes, healthcare facilities can sustain long-term efficiency and improve outcomes for future projects.
Operations, Maintenance, and Monitoring
Maintaining energy efficiency in healthcare facilities requires integrating operations, maintenance, and consistent monitoring into everyday management. Facilities that excel in sustaining energy performance make energy awareness a fundamental part of their daily decision-making and operational processes.
Maintaining Energy Performance
Ongoing staff training, combined with real-time Energy Management Systems (EMS), equips maintenance teams with the tools and knowledge to keep efficiency on track. These systems use data analytics to detect trends, such as equipment wear or seasonal shifts in efficiency, that might otherwise go unnoticed with manual checks.
"Energy Management Systems (EMS) play a pivotal role in the real-time monitoring and control of energy usage within healthcare facilities. These systems provide granular insights into consumption patterns, identify areas of high energy use, and facilitate proactive energy management."
American Hospital & Healthcare Management [3]
Preventive maintenance schedules are key to ensuring that equipment like HVAC systems, lighting controls, and building automation components operate efficiently. Regular cleaning and calibration prevent energy waste caused by neglect or deferred maintenance.
Modern monitoring devices can track electricity, water usage, and room temperatures with impressive precision. While some devices may require a higher upfront investment, their accuracy and reliability often justify the cost. For example, plug-in monitors are ideal for individual equipment, while clamp-on systems provide insights into entire building circuits or specific electrical panels. Depending on the complexity of the setup, professional installation may be necessary, so planning and budgeting for such expertise is essential.
By adopting these monitoring practices, facilities can embed a culture of energy-conscious management into their operations.
Embedding Sustainability in Facility Management
Sustainability thrives when it becomes an integral part of management practices. Incorporating energy efficiency into performance systems encourages ongoing improvement and accountability. For example, energy efficiency metrics can be included in staff evaluations and departmental budgets, ensuring everyone plays a role in achieving sustainability goals.
Building on this, improvement cycles - like monthly energy reviews - help teams spot inefficiencies early by analyzing utility bills, automation system data, and maintenance logs. These reviews provide opportunities to address anomalies before they escalate into larger issues.
Designating energy champions within departments can further reinforce energy-conscious behaviors. Acting as liaisons between their teams and facility management, these individuals cultivate a widespread commitment to energy efficiency across the organization.
Procurement decisions also play a role in sustaining efficiency. When replacing equipment or supplies, prioritizing energy-efficient options alongside cost and functionality ensures long-term gains. These efforts, paired with robust documentation and reporting systems, help track progress against established benchmarks. Regular reporting not only informs budget planning but also supports future investments in efficiency improvements.
Regular Reviews and Adjustments
Routine reviews are essential for tracking energy performance indicators and identifying deviations in usage, equipment functionality, and maintenance expenses. Seasonal adjustments, such as modifying HVAC settings or lighting schedules, ensure facilities adapt to changing weather and occupancy levels without sacrificing efficiency or patient care.
Organizations like Council Fire offer specialized expertise in energy performance reviews, helping healthcare facilities analyze complex data and uncover opportunities for optimization. Their balanced approach integrates financial planning with sustainability efforts, ensuring both cost control and environmental goals are met.
Staying up to date with technology advancements is equally important. New building automation software, monitoring devices, and control systems can enhance functionality and improve efficiency. Regularly evaluating these updates keeps facilities at the forefront of energy management.
Benchmarking performance against industry standards provides valuable context, revealing whether current practices align with best practices or need adjustment. Comparing metrics like energy use intensity against similar facilities can highlight areas for improvement.
Finally, user-friendly monitoring systems with accessible mobile or web interfaces encourage staff engagement. When data is easy to process and analyze, teams can quickly identify and address issues, ensuring continuous improvements in energy efficiency.
Conclusion and Key Takeaways
Energy efficiency in healthcare facilities goes beyond simply cutting costs - it plays a pivotal role in improving financial performance, enhancing clinical outcomes, and addressing environmental concerns. Achieving meaningful results requires teamwork across the organization, from leadership to frontline staff.
Highlights of Energy Efficiency Benefits
Reducing energy consumption leads to lower utility expenses, increased reliability of equipment, and decreased maintenance costs, which can free up resources for other facility improvements. Modern HVAC systems and advanced building automation technologies optimize energy use while ensuring precise climate control - an essential factor for patient recovery and staff productivity. Additionally, upgraded lighting systems improve visibility in critical areas while consuming less energy.
The environmental benefits are equally compelling. Lower energy usage translates to a reduced carbon footprint and contributes to cleaner air in the surrounding community, aligning with the values of patients, staff, and local stakeholders. Enhanced indoor conditions, such as better temperature consistency, improved air quality, and quieter operations, also create a more conducive healing environment, reinforcing the facility's commitment to comprehensive care.
Moving Forward with Implementation
Once the groundwork has been laid through assessments and initial steps, the focus shifts to ensuring these energy efficiencies deliver lasting value. Long-term planning is crucial to meet evolving demands and incorporate emerging technologies.
Engaging stakeholders is a cornerstone of successful implementation. Gaining buy-in from clinical teams, facility managers, financial planners, and executive leaders ensures that energy initiatives are well-supported and properly resourced. Regular updates and communication help maintain enthusiasm and encourage ongoing participation.
Expert guidance can simplify the process. Organizations like Council Fire provide valuable expertise in integrating energy efficiency with financial and operational goals. Their collaborative strategies help healthcare facilities navigate the complexities of energy management, ensuring alignment with broader objectives while maximizing both cost savings and environmental benefits.
As energy management tools and technologies continue to advance, healthcare facilities with robust practices - such as thorough monitoring, consistent maintenance, staff training, and performance evaluations - will be well-positioned to seize new opportunities and maintain leadership in energy efficiency.
Achieving optimal energy efficiency is a continuous journey. By committing to a well-rounded and deliberate approach, healthcare facilities can secure long-term financial returns, enhance patient care, and contribute positively to their communities. These efforts not only support sustainable healthcare practices but also strengthen the facility’s position as a leader in energy-conscious operations.
FAQs
What are the most affordable ways for healthcare facilities to improve energy efficiency without affecting patient care?
Healthcare facilities can take practical steps to improve energy efficiency without interfering with patient care. For instance, switching to LED lighting can significantly cut energy use while providing reliable illumination. Installing motion sensors to automate lighting and HVAC systems further reduces unnecessary energy consumption. Addressing issues like leaks in steam and water systems is another straightforward way to prevent waste.
Another effective measure is the use of variable frequency drives on equipment, which helps adjust energy use to match operational needs without sacrificing performance. These strategies are budget-friendly and simple to implement, allowing facilities to lower energy costs while maintaining a safe and comfortable environment for both patients and staff.
How can healthcare facilities improve energy efficiency without compromising indoor air quality or infection control?
Healthcare facilities can improve energy efficiency without compromising indoor air quality or infection control by using high-efficiency air filtration systems like HEPA filters or UV germicidal irradiation (UVGI). These advanced systems effectively reduce airborne pathogens while maintaining energy-efficient airflow.
Facilities can also fine-tune ventilation by adjusting outdoor air intake and limiting unnecessary air exchanges during times of low occupancy. This approach saves energy while ensuring adequate airflow, as long as the systems are thoughtfully designed, regularly monitored, and properly maintained. Routine evaluations and updates to HVAC systems are crucial to achieving the right balance between energy efficiency and safety standards.
Why are energy audits important for improving energy efficiency in healthcare facilities?
Energy audits are essential for healthcare facilities aiming to improve energy efficiency. These assessments offer a detailed examination of energy consumption, highlighting inefficiencies and creating a foundation for monitoring progress.
By uncovering precise areas where savings are possible, facilities can establish practical, measurable goals and focus on the most impactful energy-saving strategies. This approach not only lowers operational expenses but also supports better resource management and sustainability - key priorities in the energy-demanding healthcare industry.
Related Blog Posts

FAQ
01
What does it really mean to “redefine profit”?
02
What makes Council Fire different?
03
Who does Council Fire you work with?
04
What does working with Council Fire actually look like?
05
How does Council Fire help organizations turn big goals into action?
06
How does Council Fire define and measure success?


Sep 25, 2025
Ultimate Guide to Energy Efficiency in Healthcare
Sustainability Strategy
In This Article
Explore effective energy efficiency strategies for healthcare facilities that enhance patient care while reducing costs and environmental impact.
Ultimate Guide to Energy Efficiency in Healthcare
Healthcare facilities consume about 9% of the energy used by commercial buildings in the U.S., despite occupying only 4% of the total commercial floorspace. This makes energy efficiency a critical focus for cost reduction, patient care, and environmental responsibility. By upgrading systems like HVAC, lighting, and building insulation, hospitals can reduce energy use by up to 30% without compromising safety or comfort.
Key Takeaways:
Energy Audits: Identify inefficiencies and benchmark against industry standards.
Building Upgrades: Improve insulation, seal air leaks, and install energy-efficient windows.
System Optimization: Transition to LED lighting, use smart HVAC controls, and implement energy recovery systems.
Renewable Energy: Integrate solar panels, combined heat and power systems, or geothermal solutions.
Stakeholder Collaboration: Engage facility managers, medical staff, and administrators to align energy goals with operational needs.
Implementation Strategies: Minimize disruptions with phased upgrades, temporary redundancies, and rigorous system testing.
Long-term success depends on regular monitoring, preventive maintenance, and post-upgrade evaluations to ensure systems perform as planned. With proper planning and execution, healthcare facilities can achieve energy efficiency while maintaining high standards of patient care and operational reliability.
HVAC: Hospitals and health care facilities
Energy Assessment and Planning
Laying the groundwork for energy efficiency in healthcare facilities starts with thorough assessment and well-thought-out planning. These steps ensure that investments not only yield strong returns but also support the uninterrupted operations critical to patient care. The planning phase demands collaboration across various stakeholders and often benefits from expert guidance to address the unique needs of healthcare environments. Below, we explore the key components of energy audits and the role of stakeholder engagement in driving meaningful improvements.
Energy Audits and Benchmarking
In healthcare, where operations run around the clock and regulatory demands are high, energy audits are an essential tool. These audits assess facility systems by comparing their performance to design specifications or the most effective technologies available [2]. For hospitals and clinics, this evaluation is vital to achieving energy efficiency without compromising patient care.
Auditors rely on utility data, building blueprints, and system evaluations to establish a performance baseline. This baseline allows facilities to track progress, spot trends, and refine energy practices over time [2][3][5]. The potential for improvement is striking: hospitals could save up to 30% of their energy use without sacrificing comfort or safety by adopting best practices and upgrading to efficient systems [4]. This is particularly significant given that healthcare facilities in the U.S. account for about 9% of energy consumption in commercial buildings, despite occupying just 4% of the total commercial floorspace [4].
Benchmarking adds another layer of insight by comparing a facility's energy use intensity with regional and national averages. This contextual analysis highlights specific areas where improvements can be made, helping facilities prioritize their energy goals.
Stakeholder Engagement and Goal Setting
Effective energy planning hinges on the involvement of a wide range of stakeholders. From straightforward behavioral adjustments to complex system overhauls, achieving alignment among these groups is critical for success [1].
Facility managers bring operational insight and knowledge of existing systems, enabling them to identify and prioritize improvement opportunities.
Medical staff ensure that patient care remains the top priority, particularly in areas like operating rooms and intensive care units where stable conditions are non-negotiable.
Administrative leaders provide the financial backing and strategic vision to integrate energy goals with broader institutional objectives.
Setting goals for energy efficiency involves balancing ambition with practicality. Both short- and long-term objectives should be clearly defined, with mechanisms for measuring and verifying progress built into the plan. This collaborative approach ensures that all parties are aligned and ready to work toward shared outcomes.
Working with Consultants for Planning
Expert consultants can play a pivotal role in crafting effective energy strategies for healthcare facilities. Their specialized knowledge ensures that plans align with U.S. standards and industry best practices. Through detailed audits, consultants help identify opportunities for high-return investments and energy conservation [2]. They also bring a fresh perspective, often uncovering opportunities that internal teams might miss, and help avoid common pitfalls during implementation.
Organizations like Council Fire offer end-to-end support, combining financial considerations with environmental and operational goals. Their expertise helps healthcare facilities design energy strategies that improve efficiency while supporting sustainability objectives.
When choosing a consultant, healthcare organizations should prioritize firms with proven technical expertise and a track record in the healthcare sector. Deliverables such as detailed energy models, prioritized action plans, and ongoing performance monitoring should be part of the package, ensuring a clear and actionable path forward.
Key Energy Efficiency Measures
Once assessments are complete and goals are defined, the next step is implementing targeted measures in three main areas: improving the building envelope, optimizing lighting and HVAC systems, and incorporating renewable energy solutions. These steps transform planning into tangible energy savings while addressing the unique operational needs of healthcare facilities.
Building Envelope Improvements
The building envelope serves as the primary barrier against energy loss, making it a critical focus for efficiency upgrades in healthcare settings. Enhancing insulation, installing energy-efficient windows with low-emissivity coatings, and sealing gaps are practical ways to reduce HVAC demands and improve indoor comfort.
Upgrading insulation is among the most cost-effective strategies, especially when tailored to the climate zone of the facility. Better-insulated walls and roofs reduce the workload on mechanical systems, allowing them to operate more efficiently.
Air sealing is equally important. By closing gaps around penetrations, joints, and other connections, facilities can minimize energy loss and maintain precise pressure relationships - an essential factor in healthcare environments where air quality and infection control are priorities. Using the right materials for sealing ensures both energy efficiency and compliance with indoor air quality standards.
These envelope improvements work hand-in-hand with HVAC systems, enabling them to perform more effectively with reduced strain and lower maintenance requirements.
Lighting and HVAC System Optimization
Lighting and HVAC systems are major energy consumers in healthcare facilities, making their optimization a key area for improvement. The transition to LED lighting offers significant benefits, including lower energy consumption, longer lifespan, and excellent light quality. Adding controls such as occupancy sensors and daylight-responsive systems further reduces energy use in areas with variable occupancy.
For HVAC systems, upgrades can deliver substantial energy savings while maintaining the high performance required in healthcare settings. Installing variable frequency drives on motors and fans allows systems to adjust output based on real-time needs, improving efficiency. Smart building automation systems provide continuous monitoring and adjustments, ensuring optimal performance and reducing waste.
Energy recovery ventilation systems are another valuable addition. These systems capture heat and moisture from exhaust air to pre-condition incoming fresh air, which is particularly beneficial in healthcare facilities where high ventilation rates are essential for infection control.
Renewable Energy Solutions
Renewable energy solutions complement efficiency upgrades by reducing reliance on grid power and lowering operational costs. Solar photovoltaic systems, for example, can be installed on rooftops or over parking areas, aligning well with daytime energy demands. These systems often have a short payback period, thanks to reduced electricity expenses.
Other renewable options include combined heat and power (CHP) systems, which generate electricity while utilizing waste heat for space heating or hot water needs. Thermal energy storage systems, such as ice storage, allow facilities to store cooling capacity during off-peak hours and use it during peak demand. Geothermal heat pump systems leverage stable underground temperatures to provide energy-efficient heating and cooling.
To ensure these renewable systems integrate seamlessly with existing infrastructure, careful planning is essential. Coordination with backup power systems is particularly important to guarantee uninterrupted operation of critical healthcare systems.
Implementation and Quality Assurance
After thorough planning and evaluation, the next critical step in energy upgrades is executing them with minimal disruption while ensuring systems perform as intended. In healthcare settings, this phase demands precise coordination to maintain patient safety and operational continuity. Success hinges on careful planning, rigorous testing, and continuous monitoring to confirm that upgrades meet design and performance expectations.
Reducing Disruptions During Implementation
To avoid interrupting patient care, energy projects are often carried out in phases. This approach allows work to proceed in specific sections while other areas of the facility remain fully operational.
Temporary redundancies are essential for critical systems undergoing upgrades. For example, portable HVAC units can maintain climate control in patient areas while permanent systems are being updated. Scheduling non-critical upgrades during nights and weekends further minimizes disruptions, and daily staff briefings help everyone navigate temporary changes efficiently.
Clear signage and designated alternative routes ensure that staff and patients can move safely around construction zones without affecting care delivery. Emergency preparedness also becomes a top priority during this phase: backup power systems should remain fully functional, and life safety systems must be continuously monitored. Installing temporary monitoring systems provides real-time alerts if critical systems experience interruptions.
Collaboration with infection control teams is vital to maintain sterile environments during construction. Measures like negative pressure barriers, dust containment systems, and specialized ventilation are crucial for maintaining air quality in sensitive areas such as operating rooms and intensive care units.
Commissioning and Performance Verification
Commissioning is the process of validating that all systems meet their design specifications and operational requirements. This involves testing individual components before integrating them into the larger system.
Initial testing focuses on functional checks for components like motors, fans, pumps, and control devices to ensure they meet performance standards. Calibration of temperature sensors, pressure gauges, and airflow meters ensures accurate readings, which are critical for ongoing operations.
Building automation systems play a key role by continuously monitoring energy use, efficiency, and environmental conditions. Real-time data collection enables facility managers to quickly identify and address performance issues.
Staff training is another essential part of commissioning. Maintenance teams are trained on operating procedures, troubleshooting methods, and routine maintenance schedules. Detailed documentation, including operating manuals, warranty information, and maintenance plans, ensures that teams have the resources they need to manage the upgraded systems effectively.
Performance verification extends beyond initial testing. By analyzing trends over the first several months, facility managers can identify seasonal variations, usage patterns, and opportunities for system adjustments that may not have been evident during commissioning.
Post-Occupancy Evaluation for Improvement
Post-occupancy evaluations provide critical feedback on how energy efficiency measures perform under real-world conditions. Conducted 12 to 18 months after project completion, these assessments allow time for systems to stabilize and for staff to adapt to new procedures.
Energy consumption data is compared with initial projections to confirm whether efficiency goals are being met. Utility bills and automation system data offer a clear picture of actual performance. If significant deviations arise, they are investigated to determine the cause.
Indoor environmental quality is also assessed to ensure that energy upgrades haven't negatively impacted patient comfort or clinical operations. Metrics like temperature, humidity, and air quality are monitored to confirm that the facility meets required standards.
Staff feedback collected through surveys and interviews offers insights that technical data might overlook. This input often reveals small adjustments that can enhance both energy performance and user satisfaction.
The evaluation process also examines maintenance needs and operational costs. Comparing actual maintenance requirements to initial projections helps refine future planning. A cost-benefit analysis updates financial models with real-world data, providing a more accurate foundation for future energy projects.
Organizations like Council Fire bring specialized expertise to post-occupancy evaluations, helping healthcare facilities analyze performance data and identify further opportunities for system optimization. Their experience with energy and water infrastructure projects ensures a thorough assessment and actionable recommendations.
Quarterly performance reviews track key indicators, highlighting any trends that could signal equipment wear or operational changes. This ongoing evaluation helps maintain energy efficiency benefits while ensuring the facility continues to meet the high standards of patient care. By continuously refining processes, healthcare facilities can sustain long-term efficiency and improve outcomes for future projects.
Operations, Maintenance, and Monitoring
Maintaining energy efficiency in healthcare facilities requires integrating operations, maintenance, and consistent monitoring into everyday management. Facilities that excel in sustaining energy performance make energy awareness a fundamental part of their daily decision-making and operational processes.
Maintaining Energy Performance
Ongoing staff training, combined with real-time Energy Management Systems (EMS), equips maintenance teams with the tools and knowledge to keep efficiency on track. These systems use data analytics to detect trends, such as equipment wear or seasonal shifts in efficiency, that might otherwise go unnoticed with manual checks.
"Energy Management Systems (EMS) play a pivotal role in the real-time monitoring and control of energy usage within healthcare facilities. These systems provide granular insights into consumption patterns, identify areas of high energy use, and facilitate proactive energy management."
American Hospital & Healthcare Management [3]
Preventive maintenance schedules are key to ensuring that equipment like HVAC systems, lighting controls, and building automation components operate efficiently. Regular cleaning and calibration prevent energy waste caused by neglect or deferred maintenance.
Modern monitoring devices can track electricity, water usage, and room temperatures with impressive precision. While some devices may require a higher upfront investment, their accuracy and reliability often justify the cost. For example, plug-in monitors are ideal for individual equipment, while clamp-on systems provide insights into entire building circuits or specific electrical panels. Depending on the complexity of the setup, professional installation may be necessary, so planning and budgeting for such expertise is essential.
By adopting these monitoring practices, facilities can embed a culture of energy-conscious management into their operations.
Embedding Sustainability in Facility Management
Sustainability thrives when it becomes an integral part of management practices. Incorporating energy efficiency into performance systems encourages ongoing improvement and accountability. For example, energy efficiency metrics can be included in staff evaluations and departmental budgets, ensuring everyone plays a role in achieving sustainability goals.
Building on this, improvement cycles - like monthly energy reviews - help teams spot inefficiencies early by analyzing utility bills, automation system data, and maintenance logs. These reviews provide opportunities to address anomalies before they escalate into larger issues.
Designating energy champions within departments can further reinforce energy-conscious behaviors. Acting as liaisons between their teams and facility management, these individuals cultivate a widespread commitment to energy efficiency across the organization.
Procurement decisions also play a role in sustaining efficiency. When replacing equipment or supplies, prioritizing energy-efficient options alongside cost and functionality ensures long-term gains. These efforts, paired with robust documentation and reporting systems, help track progress against established benchmarks. Regular reporting not only informs budget planning but also supports future investments in efficiency improvements.
Regular Reviews and Adjustments
Routine reviews are essential for tracking energy performance indicators and identifying deviations in usage, equipment functionality, and maintenance expenses. Seasonal adjustments, such as modifying HVAC settings or lighting schedules, ensure facilities adapt to changing weather and occupancy levels without sacrificing efficiency or patient care.
Organizations like Council Fire offer specialized expertise in energy performance reviews, helping healthcare facilities analyze complex data and uncover opportunities for optimization. Their balanced approach integrates financial planning with sustainability efforts, ensuring both cost control and environmental goals are met.
Staying up to date with technology advancements is equally important. New building automation software, monitoring devices, and control systems can enhance functionality and improve efficiency. Regularly evaluating these updates keeps facilities at the forefront of energy management.
Benchmarking performance against industry standards provides valuable context, revealing whether current practices align with best practices or need adjustment. Comparing metrics like energy use intensity against similar facilities can highlight areas for improvement.
Finally, user-friendly monitoring systems with accessible mobile or web interfaces encourage staff engagement. When data is easy to process and analyze, teams can quickly identify and address issues, ensuring continuous improvements in energy efficiency.
Conclusion and Key Takeaways
Energy efficiency in healthcare facilities goes beyond simply cutting costs - it plays a pivotal role in improving financial performance, enhancing clinical outcomes, and addressing environmental concerns. Achieving meaningful results requires teamwork across the organization, from leadership to frontline staff.
Highlights of Energy Efficiency Benefits
Reducing energy consumption leads to lower utility expenses, increased reliability of equipment, and decreased maintenance costs, which can free up resources for other facility improvements. Modern HVAC systems and advanced building automation technologies optimize energy use while ensuring precise climate control - an essential factor for patient recovery and staff productivity. Additionally, upgraded lighting systems improve visibility in critical areas while consuming less energy.
The environmental benefits are equally compelling. Lower energy usage translates to a reduced carbon footprint and contributes to cleaner air in the surrounding community, aligning with the values of patients, staff, and local stakeholders. Enhanced indoor conditions, such as better temperature consistency, improved air quality, and quieter operations, also create a more conducive healing environment, reinforcing the facility's commitment to comprehensive care.
Moving Forward with Implementation
Once the groundwork has been laid through assessments and initial steps, the focus shifts to ensuring these energy efficiencies deliver lasting value. Long-term planning is crucial to meet evolving demands and incorporate emerging technologies.
Engaging stakeholders is a cornerstone of successful implementation. Gaining buy-in from clinical teams, facility managers, financial planners, and executive leaders ensures that energy initiatives are well-supported and properly resourced. Regular updates and communication help maintain enthusiasm and encourage ongoing participation.
Expert guidance can simplify the process. Organizations like Council Fire provide valuable expertise in integrating energy efficiency with financial and operational goals. Their collaborative strategies help healthcare facilities navigate the complexities of energy management, ensuring alignment with broader objectives while maximizing both cost savings and environmental benefits.
As energy management tools and technologies continue to advance, healthcare facilities with robust practices - such as thorough monitoring, consistent maintenance, staff training, and performance evaluations - will be well-positioned to seize new opportunities and maintain leadership in energy efficiency.
Achieving optimal energy efficiency is a continuous journey. By committing to a well-rounded and deliberate approach, healthcare facilities can secure long-term financial returns, enhance patient care, and contribute positively to their communities. These efforts not only support sustainable healthcare practices but also strengthen the facility’s position as a leader in energy-conscious operations.
FAQs
What are the most affordable ways for healthcare facilities to improve energy efficiency without affecting patient care?
Healthcare facilities can take practical steps to improve energy efficiency without interfering with patient care. For instance, switching to LED lighting can significantly cut energy use while providing reliable illumination. Installing motion sensors to automate lighting and HVAC systems further reduces unnecessary energy consumption. Addressing issues like leaks in steam and water systems is another straightforward way to prevent waste.
Another effective measure is the use of variable frequency drives on equipment, which helps adjust energy use to match operational needs without sacrificing performance. These strategies are budget-friendly and simple to implement, allowing facilities to lower energy costs while maintaining a safe and comfortable environment for both patients and staff.
How can healthcare facilities improve energy efficiency without compromising indoor air quality or infection control?
Healthcare facilities can improve energy efficiency without compromising indoor air quality or infection control by using high-efficiency air filtration systems like HEPA filters or UV germicidal irradiation (UVGI). These advanced systems effectively reduce airborne pathogens while maintaining energy-efficient airflow.
Facilities can also fine-tune ventilation by adjusting outdoor air intake and limiting unnecessary air exchanges during times of low occupancy. This approach saves energy while ensuring adequate airflow, as long as the systems are thoughtfully designed, regularly monitored, and properly maintained. Routine evaluations and updates to HVAC systems are crucial to achieving the right balance between energy efficiency and safety standards.
Why are energy audits important for improving energy efficiency in healthcare facilities?
Energy audits are essential for healthcare facilities aiming to improve energy efficiency. These assessments offer a detailed examination of energy consumption, highlighting inefficiencies and creating a foundation for monitoring progress.
By uncovering precise areas where savings are possible, facilities can establish practical, measurable goals and focus on the most impactful energy-saving strategies. This approach not only lowers operational expenses but also supports better resource management and sustainability - key priorities in the energy-demanding healthcare industry.
Related Blog Posts

FAQ
What does it really mean to “redefine profit”?
What makes Council Fire different?
Who does Council Fire you work with?
What does working with Council Fire actually look like?
How does Council Fire help organizations turn big goals into action?
How does Council Fire define and measure success?


